Discovering new genes responsible for DSDs
Discovering new genes responsible for DSDs is a Research Project for the Sex Development Research Group, under the Centre for Endocrinology and Metabolism.
Project Leader
Disorders/Differences of Sex Development (DSD) encompass a very large spectrum of phenotypes that range from hypospadias to completely masculinised or feminised genitalia with a discordant karyotype. In the aggregate, DSD have an estimated incidence of about 1%. Reaching a genetic diagnosis can significantly impact on management, gender assignment, genetic counselling, prognostic prediction of fertility, and the risk assessment of tumour development. However, the highly heterogeneous nature, as well as the overlap of phenotypes, of this group of conditions make a genetic diagnosis a challenge. Despite much progress in the past 30 years, the molecular basis in 65% of the patients with DSD remains unknown.
The long-term objective is to identify and investigate novel sex-determining genes and to break through the current diagnostic impasse. We anticipate that the whole genome sequencing (WGS) of well-phenotyped patients with DSD will radically transform our understanding of the development and diagnosis of DSD. The search for molecular mechanisms involved in DSD has mainly focused on the coding part of the genome so far. Expanding the search window towards the non-coding genome will result in new mechanistic pathogenetic insight that will have an impact upon the knowledge of the process of sex development that currently is not fully understood.
We will take advantage of access to the Monash Children’s Hospital and the Australian Paediatric Endocrine Group (APEG) to recruit 46,XY GD patients and families per year. We will also utilise a large NIH-funded Registry and Biobank (the DSD Translational Research Network, CIB Vilain is a co-PI) to source 5 46,XY GD patients per year.
Professor Harley has impacted the DSD field through the identification and validation of genetic variants in many DSD genes including SRY, SOX9, WNT4, DAX1, SF1 and ATRX with landmark papers in Science, Nature Genetics, The Lancet DE, Genome Biology, PLoS Biology, JCI (2), EMBO (2), NAR (3), PNAS, and by CIB in NEJM, The Lancet, Nature, Nature Genetics (2), AJHG (2), JAMA, Genome Research and PNAS (2). The expertise of Professor Harley in modelling DSD variants in cellular and animal models places us in a unique position allowing for the best possible interpretation of data generated by WGS and other genomic approaches.
In most 46,XY DSD cases it is not possible to identify a causative mutation, making genetic counselling difficult and potentially hindering optimal treatment. Whole-genome analysis (with A. Sinclair, MCRI) of a 46,XY DSD patient that presented at birth with ambiguous genitalia revealed a heterozygous deletion within the WWOX gene, inherited from the mother, supporting a role for WWOX in human gonad development.
In a multicentre study including PHI led by P. Thomas (U. Adelaide), scientists accidentally turned on Sox3, a gene normally found in the brain, in the gonads leading to xx male mice. Analogously, in three male patients with 46,XX DSD, we also identified genomic rearrangements within the SOX3 regulatory region, a relatively common cause of XX DSD in cases lacking the SRY gene.
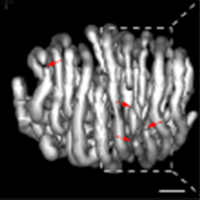
In a collaboration with S. Lyonnet (Necker Hospital, Paris) genome wide analysis of DSD patients identified a testis enhancer region of the SOX9 gene located far upstream of the SOX9 promoter. Gain or loss of this region was associated with 46,DSD or 46, XY DSD respectively. The development of high-resolution CGH microarray is the next powerful tool needed to overcome these difficulties and will likely produce new information on human gonadal development. Array Comparative Genomic Hybridization (CGH) measures DNA copy number differences between a reference genome and a sample genome. Using whole-genome array CGH, we can measure copy number differences in DNA across entire genomes.
Given the complexity of phenotypes to be analysed by CGH, it is crucial to narrow down the patient numbers to be analysed to very carefully diagnosed patients.
We are currently screening several XY female patients, which harbour a normal SRY gene, for copy number differences across their entire genome.