Endometriosis
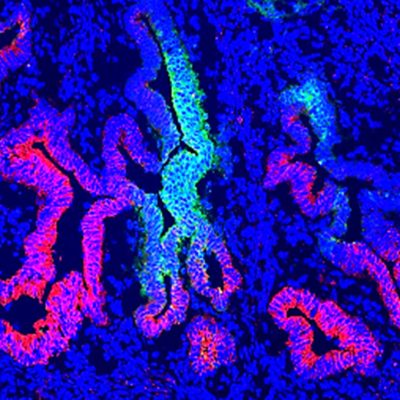

Feature image | Human endometrial epithelial progenitor cells
How medical research is helping people with endometriosis
Endometriosis can have a debilitating effect on women’s lives. It can take six and a half years before a woman gets a diagnosis and, because the cause is unknown, there is no effective treatment or cure.
Hudson Institute is leading medical research into women’s reproductive health and is home to some of the world’s top scientists in endometrial research. Our scientists researchers are working towards finding the cause of endometriosis to improve treatment, management and diagnosis. By unveiling the science behind the disease, our researcher’s goals are to
- Develop a non-invasive early diagnostic test
- Investigate the potential of non-surgical and non-hormonal treatment options
- Improve detection of infertility in women with the disease.
Endometriosis research projects
Role of endometrial stem cells in endometriosis

New treatment targets for endometriosis

A non-invasive diagnostic for endometriosis and adenomyosis

Investigating the link between endometriosis and infertility

Real life endometriosis stories
Nicole’s story | Bianca’s story | Evelyn’s story | Kat’s story | Bridget’s story
Endometriosis fact sheet, symptoms, diagnosis
What is endometriosis?

Endometriosis is a chronic inflammatory condition where tissue fragments similar to the womb lining attach to other organs and grow into lesions outside the uterus.
The lesions remain responsive to female reproductive hormones that trigger menstruation, and as a result may bleed during menstruation, causing debilitating symptoms including back pain, heavy menstrual bleeding, bladder problems, bowel problems and infertility.
See the fact sheet to learn more.
What is adenomyosis?
Adenomyosis is a condition affecting an estimated two per cent of women, where cells that normally line the uterus also grow in the muscle wall of the uterus. Symptoms include abnormal or heavy menstrual bleeding and painful periods.
Symptoms incude
- Pelvic and back pain
- Heavy menstrual bleeding
- Bladder problems, nausea
- Bowel problems
- Pain during sex
- Infertility. Read about Nicole’s story.
Stages
The disease is often classified as minimal, mild, moderate or severe, or from stage I to stage IV. There is no early detection test for endometriosis.
Cause

The cause of the the condition is a key question facing scientists today. Hudson Institute researchers are working on the hypothesis that the disease is caused by retrograde menstruation, where menstrual fluid containing cells that initiate endometriosis flows backward through the uterus, out the fallopian tubes and into the pelvic cavity. These cells somehow evade the immune system, attach to organs and form lesions.
One in 9
At least one in 9 girls and women and those assigned female at birth are affected by endometriosis in Australia, making it as common in women as asthma or diabetes.
Hudson Institute researchers are working towards finding the cause to improve treatment, management and diagnosis for the 176 million women worldwide and 560,000 in Australia who have the condition.
Endometriosis diagnosis

There is often a long delay in diagnosing endometriosis, and women can wait six and half years to receive a correct diagnosis. A keyhole surgical procedure called a laparoscopy is the main method used to diagnose endometriosis. However, some types of endometriosis may be diagnosed through an ultrasound or MRI.
Endometriosis treatment

There is no cure and no effective treatment. Current treatment and management options include hormonal therapies and surgery to remove lesions to reduce pain and improve fertility.
Hormonal treatments (oral contraceptive pill, or progestins such as an intrauterine device (IUD) may be used to suppress the growth of endometrial tissue and stop irregular bleeding.
Lesion excision, performed via laparoscopy, may be required to remove endometriosis lesions.
In some cases, a hysterectomy may be required to remove severe endometriosis. Pain and anti-inflammatory medication may be prescribed or used to treat and reduce pain and symptoms. Consult your medical professional for advice on treating and managing endometriosis.
Endometriosis fertility and pregnancy

Around one third of women with endometriosis will have trouble falling pregnant.
Symptoms don’t always correlate with the severity of the disease. This means some women are asymptomatic and may only be diagnosed incidentally when they start trying to have children.
Importantly, not all women with the condition experience infertility, and many women have children either before or after their diagnosis.
Infertility can be caused by scarring and distortion of the fallopian tubes and ovaries, reduced egg quantity and quality caused by damage to eggs in the ovaries, damage to or blockage of the fallopian tubes, or lesions that become adherent to the uterus, bowel or pelvic wall.
Keep up-to-date with endometriosis research via the ENDO newsletter.
Endometriosis news
Collaborators
- University of Queensland
- Monash Health
- Epworth Hospital
- Monash University, Department of Obstetrics and Gynaecology
Keep up-to-date with our latest discoveries




 Dr Fiona Cousins is aiming to develop new endometriosis treatments that focus on the immune system.
Dr Fiona Cousins is aiming to develop new endometriosis treatments that focus on the immune system.
