Reducing stillbirth – roll-out of national program
By Hudson Institute communications. Reviewed by Associate Professor Miranda Davies-Tuck
Health services across Australia will have access to new clinical guidelines that will help prevent stillbirth, thanks to a recently awarded postdoctoral fellowship from the Centre for Research Excellence in Stillbirth.

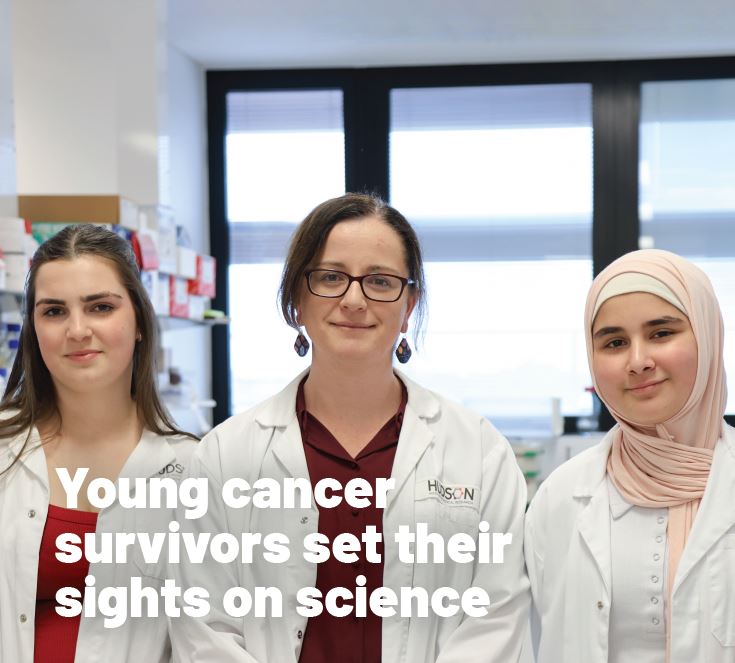
Hudson Institute’s Dr Miranda Davies-Tuck has been awarded the fellowship to roll-out, evaluate and expand guidelines she developed in 2017 that provide clinicians with new parameters for fetal surveillance in late pregnancy. To date, her new guidelines have only been implemented at one health service in Melbourne, and this funding will see them taken Australia-wide.
The project aims to reduce the disproportionately high rate of stillbirth encountered by south Asian mothers due to biological placental differences. These differences make them more susceptible to stillbirth than women born in Australia, New Zealand, Europe or South East Asia.
Most at-risk mothers for stillbirth
Dr Davies-Tuck’s work has identified that a mother’s ethnicity is an independent risk factor for stillbirth at term. Prior to her work, a mother’s country of birth was considered a risk factor for stillbirth only in the context of migration and socioeconomic factors.
Her study identified why this risk is higher in south Asian women, finding that the placenta ‘ages’ more rapidly in certain ethnic groups, leading to not only an increased risk of stillbirth in the term period overall, but an increased risk at earlier gestations not previously considered.
The finding meant an overhaul of clinical guidelines for fetal surveillance in late pregnancy was needed. Dr Davies-Tuck translated her findings into new guidelines, and oversaw the implementation of them at Victoria’s largest maternity service, Monash Health.
Normally women undergo monitoring of their baby via an ultrasound from 41 weeks gestation, the new guidelines commence this monitoring from 39 weeks for women of South Asian background.
Funding the roll-out of these guidelines
At present the guidelines have only been implemented at Monash Health. Since the guidelines have been introduced, Monash Health has halved the rate of stillbirth at term for south Asian women, bringing the rate of term stillbirth in line with other women at the service.
Dr Davies-Tuck is now building on this work to ensure all health services across Australia have access to the new clinical guidelines through the national safer baby bundle collaboration.
She is also working on ways to reduce stillbirth in other groups at high risk and improving the identification and detection of which babies are most at risk to optimise timing of birth to prevent stillbirth.
“The guidelines have changed clinical care of south Asian women at Monash Health, which equates to around 3000 women per year.
“The fact we have seen no stillbirths in south Asian women after 39 weeks onwards since they were introduced is very promising, and shows the impact these guidelines can have as they are taken Australia-wide.”
“I feel really grateful for the support of the Centre for Research Excellence in Stillbirth to continue to collaborate with them to improve care and reduce the rates of stillbirth,” she said.
Stillbirth facts
- Stillbirth is defined as the birth of a baby without signs of life after 20 weeks’ gestation
- In Australia, six babies are stillborn every day
- The rate of stillbirth has not improved in the last two decades, despite improvements in medical care
- According to the most recent Lancet stillbirth series, Australia ranks 15 among high-income countries
- South Asian born mothers are 27 per cent more likely to experience stillbirth than Australian born mothers
- Women born in South Asia, the Middle East and Africa were more likely to have a late-term stillbirth (after 37 weeks’ gestation) than women born in Australia, New Zealand, Europe or South East Asia.
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”