Childhood Cancer Program

Some childhood cancers have either no treatment available, or what is available hasn’t improved for more than forty years.
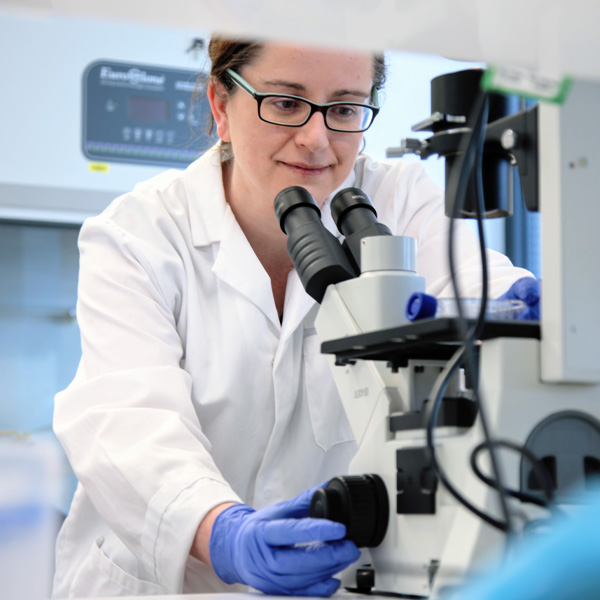
These rare, low-survival, difficult-to-treat childhood cancers are among the specialities of Hudson Institute researchers.
Each year almost 1,000 Australian children are diagnosed with childhood cancer and 5,600 are undergoing treatment.
Despite significant improvements in overall survival rates over the past 50 years, cancer remains the leading disease-related cause of death among Australian children.
The pharmaceutical industry’s limited focus on developing new treatments for paediatric cancers stems from their comparatively low incidence relative to adult cancers.
Some rare childhood cancers have no treatments available. In the last 40 years, 500 adult cancer drugs were approved in the United States, contrasting with only 12 for childhood cancers. The development of more targeted and less toxic treatments for children with cancer is imperative to improve survival rates and reduce long-term treatment-related side effects.
Our Childhood Cancer Research Programs aim to improve survival rates and long-term health outcomes for children with cancer by mitigating the detrimental effects of aggressive treatments on their developing bodies.
Leadership and goals
A world leader in the field of paediatric cancer research, Hudson Institute’s multidisciplinary team of researchers and clinicians have the following primary objectives
- Developing more precise treatments to improve childhood cancer long-term prognosis, survival rates, and long-term health outcomes.
- Fostering local, national, and international partnerships to build capacity and sustainability in paediatric cancer research.
- Advancing the understanding of cancer biology through cutting-edge research, focusing on the unique genetic and molecular profiles of paediatric cancers.
- Translating research into clinical practice by facilitating the implementation of research findings into clinical trials for paediatric cancer patients.
- Engaging in advocacy and education to raise awareness about the unique challenges of paediatric cancer and to secure funding and policy support for ongoing research and treatment initiatives.
In Australia, more than 1,000 children and adolescents are diagnosed with cancer each year.
Cancer kills three children every week in Australia – more than any other disease.

Almost half of all children diagnosed with cancer in Australia are aged 0-4 years old.

Next Generation Precision Medicine Program
The Next Generation Precision Medicine Program aims to significantly improve the treatment, survival and quality of life for children with cancer, with a special focus on brain cancer.
Learn more

AYA Sarcoma Program
Our sarcoma program includes both clinical and discovery research projects utilizing a broad range of patient tissue, in vitro and in vivo preclinical models, and techniques.
Learn more

Immunotherapy Program
Childhood cancer poses a significant scientific and medical challenge, and within this field, immunotherapy and cancer vaccines emerge as promising, less toxic treatment options.
Learn more
Acute Myeloid Leukemia Program
Our childhood AML program aims to identify critical mechanism underpinning AML development, relapse and therapy resistance.
Learn more

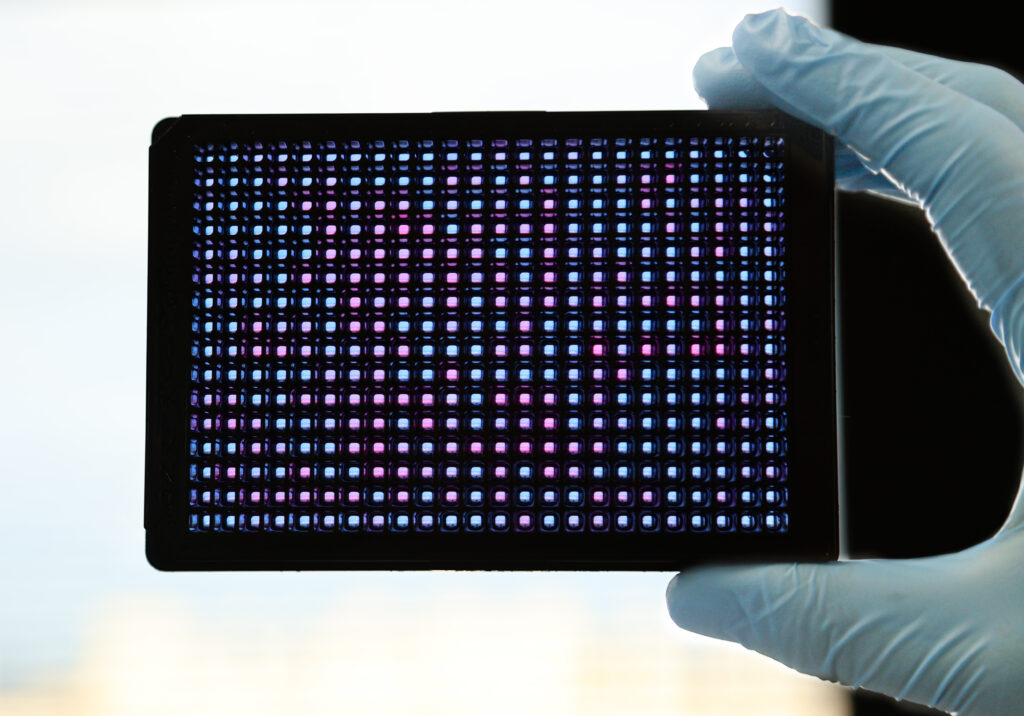
Advanced Informatics program
The Advanced Informatics program develops and applies state-of-the-art computational approaches to rapidly screen samples of the most challenging paediatric cancers against thousands of genetic alterations for potential therapeutic vulnerabilities.
Learn more
Childhood Cancer Model Atlas
The Childhood Cancer Model Atlas (CCMA), housed at Hudson Institute’s Centre for Cancer Research, is the world’s largest collection of over 400 high-risk paediatric cancer cell lines. This unique and open-source repository was established through the collaboration of more than 50 leading cancer research institutes, universities, and academic medical centres worldwide.
Monash Children Cancer Biobank and Living Biobank
The Monash Children’s Cancer Biobank was established in 2011 and is collaboratively operated at the Centre for Cancer Research at Hudson Institute, and by Monash Children’s Cancer Centre. Since 2017, the biobank has expanded to include a Living Biobank, a cutting-edge resource that features patient ‘avatar’ models. These models faithfully replicate the patient’s original tumour and include cell lines, organoids, and patient-derived xenografts (PDXs).
Publication highlights
2024

2023

2022

2021

2020

2019

2017

2016

2014

2013

2012

Program leads
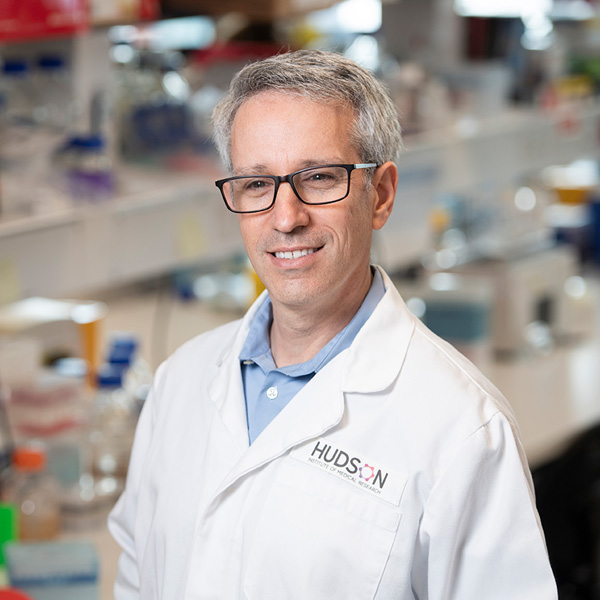
Professor Ron Firestein, Centre Head, Centre for Cancer Research, Lead Next generation precision medicine program
Associate Professor Jason Cain, Research Group Head Sarcoma program
Associate Professor Pouya Faridi, Research Group Head Cancer immunotherapy program
Dr Catherine Carmichael, Research Group Head Childhood myeloid leukemia program
Dr Xin (Claire) Sun, Advanced informatics program
Program operations
Naama Neeman, Head of Program Operations
Laboratory operations
Gilu Abraham, Laboratory Manager
Research team
Dr Paul Daniel, Senior Postdoctoral Research Fellow
Dr Terry Lim, Postdoctoral Scientist
Dr Hanbyeol Lee, Postdoctoral Scientist, Paediatric Brain Cancer
Dr Yichen Zhou, Postdoctoral Scientist, Combinatorial CRISPR Technology
Dr Farnaz Fahimi, Postdoctoral Scientist
Dr Gabriel Goncalves, Postdoctoral Scientist
Dr Shazia Adjumain, Postdoctoral Scientist, Functional Genomics – funded by Robert Connor Dawes Foundation
Dr Danxi Zhu, Postdoctoral Scientist
Dr Tima Shamekhi, Postdoctoral Scientist
Dr Ava Faridi, Grant and manuscript writing
Yuxin (Sally) Sun, Cooper Rice-Brading Foundation – Sarcoma Research Specialist
Dr Steve Lin, Research Assistant
Jingjing Zhao, Paediatric cancer model specialist – funded by Lindonlight Collective
Nivedhitha Selvakumar, Research Assistant
Jennie Do, Research Assistant
Melissa Loi, Research Assistant
Samiksha Dhananjay, Research Assistant – volunteer
Eliana Firestein, Research Assistant – volunteer
Biobanking and cell culture specialists
Dr Nicole Chew, Senior Organoid Specialist – funded by Lindonlight Collective
James Cooper, Research Assistant, Patient Model Specialist
Wan Lin Chin, Junior Research Assistant
Bioinformatics researchers
Isaac Woodhouse, Senior Bioinformatician
Vincent Xue, Bioinformatician
Vikesh Ajith, Bioinformatics Data Engineer
Xinyi Guo, Research Assistant
Yiwen Guan, Junior Research Assistant
Ishika Mahajan, Volunteer
Clinical staff
Dr Lakshmi (Priya) Sundaravel, Paediatric Fellow, The Royal Children’s Hospital
Dr Leanne Super, Paediatric Oncologist, The Royal Children’s Hospital and Monash Children’s Hospital
Students
Grace Huang, PhD Student
Dr Nataliya Zhukova, PhD Student
Dingyin Sun, PhD Student
Dr Elise Young, PhD Student
Barnaby Kelly, PhD Student
Lynda Truong, PhD Student
Nurfarhanah (Farhanah) Syed Sulaiman, PhD Scholar
Samitha Amarapathy, PhD student, Faculty of IT, Monash University
Mersedeh Shayan, PhD student
Yan Lim, PhD Student
Menghan Luo, PhD student – Ryley Kemp Scholar, funded by Isabella and Marcus Foundation
Neksha Batta, PhD student – Monash Biomedicine Discovery Institute, Monash University
Eleanor McLean, Honours Student
Erin Lin, Research Intern
Aaron Wong, Intern student
Karyn Tjahyadi, Visiting Student
Abigail Yoel, Visiting Student
Isabella Buchner, Visiting Student
The Childhood Cancer Program is conducted in collaboration with more than 50 leading cancer research institutes, universities, and academic medical centres worldwide.
National
- Centre for Cancer Biology, SA
- Flinders University, SA
- Monash Children’s Hospital, VIC
- Monash University, VIC
- Murdoch Children’s Research Institute, VIC
- Peter MacCallum Cancer Centre, VIC
- QIMR Berghofer Medical Research Institute, QLD
- Queensland Children’s Tumour Bank, QLD
- The Alfred, VIC
- The Kids Research Institute Australia, WA
- The Royal Children’s Hospital Melbourne, VIC
- The Royal Melbourne Hospital, VIC
- The Sydney Children’s Hospitals Network, NSW
- The University of Melbourne, VIC
- The University of Queensland, QLD
- The Walter and Eliza Hall Institute, VIC
- University of Newcastle, NSW
- Zero Childhood Cancer, NSW
- Children’s Medical Research Institute, NSW
- Hunter Medical Research Centre, NSW
- St. Vincent’s Hospital Melbourne, VIC
International
- American Type Culture Collection (ATCC), United States
- Bambino Gesù Children’s Hospital, Italy
- Boston Children’s Hospital, United States
- Chidren’s Hospital of Philadelphia, United States
- Childhood Cancer Repository, United States
- Children’s Brain Tumour Network (CBTN), United States
- Children’s Hospital Los Angeles, United States
- Children’s Hospital Zurich, Switzerland
- Children’s National Hospital, United States
- Chordoma Foundation, United States
- Dana-Farber Cancer Institute, United States
- Dayton Children’s, United States
- Duke University, United States
- Fred Hutchinson Cancer Center, United States
- German Cancer Research Center (DKFZ), Germany
- Hopp Children’s Cancer Center Heidelberg (KiTZ), Germany
- Johns Hopkins University, United States
- KK Women’s and Children’s Hospital, Singapore
- Leibniz Institute DSMZ, Germany
- Life Technologies, United States
- McGill University, Canada
- Merck, United States
- NIBIOHN Japanese Collection of Research Bioresources (JCRB) Cell Bank, Japan
- Princess Máxima Center for Pediatric Oncology, Netherlands
- Sant Joan de Déu Barcelona Children’s Hospital, Spain
- Spanish National Cancer Research Center (CNIO), Spain
- St. Jude Children’s Research Hospital, United States
- Stanford University, United States
- The Hospital for Sick Children (SickKids), Canada
- The Institute of Cancer Research, UK
- University of Calgary, Canada
- University of California San Francisco, United States
- University of Cambridge, UK
- University of Colorado, United States
- University of Lübeck, Germany
- University of Michigan, United States
- VU University Medical Center, Netherlands
The Childhood Cancer Program acknowledges the support of
Funders
- Australian Communities Foundation
- Australian Lions Childhood Cancer Research Foundation
- Cancer Australia
- Children’s Cancer Foundation
- Children’s Cancer CoLab
- Cooper Rice-Brading Foundation
- Isabella and Marcus Foundation
- Medical Research Future Fund
- Monash Partners Comprehensive Cancer Consortium
- My Room
- Robert Connor Dawes Foundation
- Run DIPG
- The Kids’ Cancer Project
- Tour de Cure
- Victoria State Government
- Victorian Cancer Agency
Patient and family advisors play a crucial role in shaping our childhood cancer research program by bringing invaluable insights from their personal experiences with childhood cancer.
Our advisors include caregivers of children who are currently undergoing treatment, caregivers of those who have passed away from childhood cancer and survivors of childhood cancer (or their carers). These individuals provide vital recommendations that guide our research efforts, ensuring that the perspectives of patients and families are incorporated into every stage of planning, delivery, and evaluation. They also offer advice on how to effectively communicate our research outcomes to the broader community. This collaborative approach enhances our mission of fostering partnerships, developing precise treatments, and improving both survival rates and long-term health outcomes for childhood cancer patients.

Courtney Baglin
Childhood and AYA Sarcoma program
Immunotherapy program
Next generation precision medicine

Monique Boggia
Next generation precision medicine
Andrea Boon
Leukaemia program

Prof Tracey Danaher
Next generation precision medicine
Advanced informatics program

Nader Eloshaiker
Leukaemia program

Lucy Francazio
Leukaemia program

Dr Rebecca Goldstein
Next generation precision medicine
Advanced informatics program

Claire Josefsson
Leukaemia program
Advanced informatics program

Leesa Kerr
Childhood and AYA Sarcoma program
Immunotherapy program
Next generation precision medicine

Taylah Miranda
Leukaemia program

Nelly Mohibi
Childhood and AYA Sarcoma program
Immunotherapy program
Next generation precision medicine

Virginia Rea
Next generation precision medicine
Jen Rooney
Next generation precision medicine
Advanced informatics program

Dr Lori Rubinek
Next generation precision medicine

Andrea Valvo
Leukaemia program

Tianna Valvo
Leukaemia program

Anita Watts
Childhood and AYA Sarcoma program
Immunotherapy program
Next generation precision medicine