Placental stem cells may protect against effects of pre-term lung disease
By Hudson Institute communications
A team of researchers at The Ritchie Centre, Hudson Institute of Medical Research has published further evidence to support the use of placental stem cells to protect newborn babies against the debilitating preterm lung disease, bronchopulmonary dysplasia (BPD), and its severe lifelong impacts.
In a first, the team, led by Associate Professor Tim Moss, showed in pre-clinical models that injecting amnion epithelial cells into the blood stream soon after birth could reduce injury to the preterm newborn’s lungs.
The findings of the study are published in PLOS One.
“Many preterm babies have problems breathing at birth because their lungs are immature. Some need help breathing, which can damage their lungs and contribute to long term lung disease. We showed that these cells reduce injury to the lungs when newborns require breathing support,” A/Prof Moss said.
“Ongoing breathing support for preterm babies amplifies lung injury. It’s like turning up the volume knob on your stereo. The cells we are investigating reduce the injury. They stop the stereo from getting too loud,” he said.
A specific type of lung disease: Bronchopulmonary dysplasia
Many pre-term babies can’t breathe properly without breathing support. This support saves lives but can also contribute to a type of preterm lung disease called bronchopulmonary dysplasia (BPD).
In 2013, 792 babies developed BPD in Australian and New Zealand neonatal intensive care units, and 29 of these babies (around 3.6 per cent) died due to complications arising from the disease. Babies that survive BPD may have life-long lung disease and deficits in brain function.
“There is currently no treatment for BPD and our goal is to develop a cell therapy to treat or prevent this lung disease and thereby improve the quality of life for preterm babies,” said A/Prof Moss.
Amnion epithelial cells are stem-like cells that are taken from a healthy amniotic membrane, part of the placenta that is discarded after birth.
Researchers from The Ritchie Centre at the Hudson Institute are pioneering research into these highly-potent and regenerative cells in a range of diseases affecting newborn and preterm babies.
Next stage: collaboration with University of Western Australia
“We have funding from the National Health and Medical Research Council to fund our pre-clinical studies, using research facilities at the University of Western Australia (UWA) supported by the NHMRC Preterm Infants Centre of Research Excellence. All of this has led to a dual PhD program between Monash University, Hudson Institute and the University of Western Australia (UWA),” A/Prof Moss said.
“We are using the best pre-clinical models of neonatal intensive care. This ensures relevance to clinical practice and facilitates the translation of our experimental findings,” he said.
A/Prof Moss’ research group investigates how exposure to infection and inflammation in utero alters development of the fetus to affect health after birth, and the group is studying ways to treat or prevent inflammation and its effects.
A/Prof Tim Moss is a developmental physiologist and an expert in perinatology. He is also a Board Member of the international Fetal and Neonatal Physiological Society and the Perinatal Society of Australia and New Zealand.
BPD Explainer | A common preterm disease without a cure
Pre-term babies’ immature lungs are often unable to cope with the essential and life-saving respiratory support they are placed on in hospital.
Up to 60 per cent of preterm babies will develop BPD, an inflammatory lung disease that causes severe injury to the lung tissue and prevents normal lung growth, soon after birth. The more premature a baby is at birth, the higher the risk of BPD. There is currently no safe and effective treatment.
BPD affects the alveoli, the tiny sacs in the lungs that enable the entry of oxygen into the bloodstream, and the clearance of carbon dioxide from the body.
Babies with BPD often suffer severe lifelong complications, including impaired neurodevelopment, and they are highly susceptible to airway infections that may lead to death. As a result, some of these babies will require ongoing medical care into childhood, or for some, even into adulthood.
BPD facts
- Almost 1 in 10 babies in Australia are born premature.
- Up to 60 per cent of preterm babies will develop BPD.
What is stem cell therapy?
Stem cell therapy is a treatment that uses stem cells to replace or repair cells or tissues that are damaged. The stem cells might be put into the blood, or transplanted directly into the damaged tissue. These transplants can be from the patient’s own cells or from a donor.
Contact us
Hudson Institute Communications
t: + 61 3 8572 2697
e: communications@hudson.org.au
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
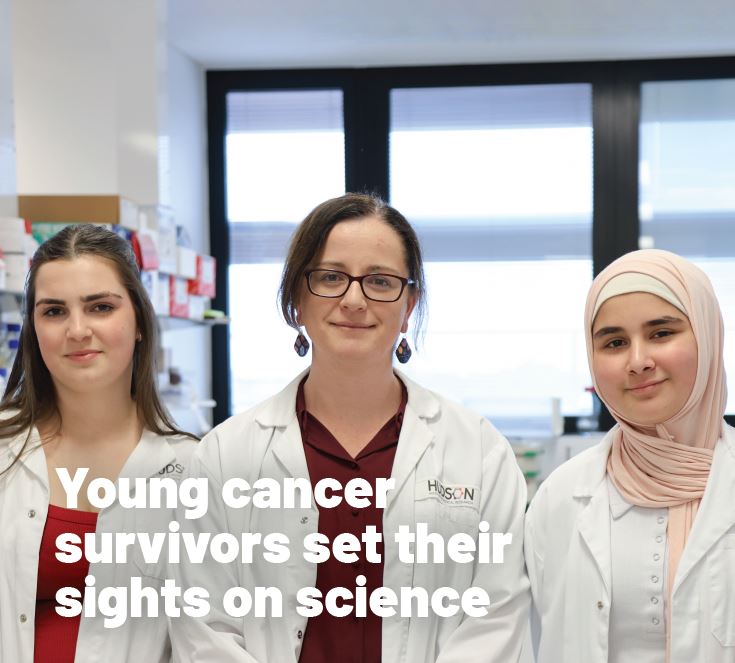
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”