Acute myeloid leukaemia program
Identifying critical mechansms underpinning AML development, relapse and therapy resistance.
Overview
Lead Researcher | Dr Catherine Carmichael
Acute myeloid leukaemia (AML), one of the most aggressive and fast-growing leukaemia subtypes, has a poor prognosis. While AML accounts for 20% of childhood leukaemia diagnoses, it causes nearly half of all leukaemia deaths. Approximately 40% of Australian children diagnosed with AML will relapse or not respond to treatment, with many of these children ultimately succumbing to their disease.
Current AML treatments include high-dose chemotherapy and bone marrow transplant. While high dose chemotherapy can induce remission in most patients, it is extremely toxic and results in significant acute and chronic (long-term) health impacts. Despite achieving remission, chemotherapy resistance and subsequent disease relapse is common. A bone marrow transplant is often the only possibility of cure for a child with relapsed AML; however, this also carries significant risk, including mortality.
For the 60-70% of children with AML who ultimately survive, many endure lifelong side effects from the high-dose chemotherapy and transplant pre-conditioning treatment, including
- Cardiovascular disease
- Endocrine disorders
- Cognitive and developmental issues
- Increased risk of secondary cancers
- Infertility
- Nerve pain.
These devastating side effects can significantly impact the ongoing quality of life for children – for years and even decades after their treatment for AML ends.
While intensive chemotherapy and improvements in supportive care have led to increased survival rates, the development of new therapeutic strategies has remained largely stagnant, with only one new drug clinically approved for use in children in the past 20 years. There is an urgent need to develop new non-chemotherapeutic or reduced toxicity treatments with greater curative potential.
The challenge for childhood AML researchers is a lack of good AML models that faithfully recapitulate the disease. A strong reliance on adult AML models, which overlook key genetic and biological differences in children, has impaired researchers’ ability to identify new therapies specifically targeting childhood AML. Developing innovative new childhood AML models will facilitate direct discovery of key disease mechanisms and leukaemia cell weaknesses that can be targeted therapeutically. Developing improved ways to treat children with AML could transform their survival rates and ultimately improve their long-term outcomes and quality of life.
Goals
To develop childhood AML cell models that enable
- Identification of key mechanisms of AML development, relapse and therapy resistance
- Large-scale genetic and chemical screening for new drug targets and therapies
- Global collaboration through model sharing for high-throughput genetic and drug screening to accelerate new therapeutic development.
AML Program Projects
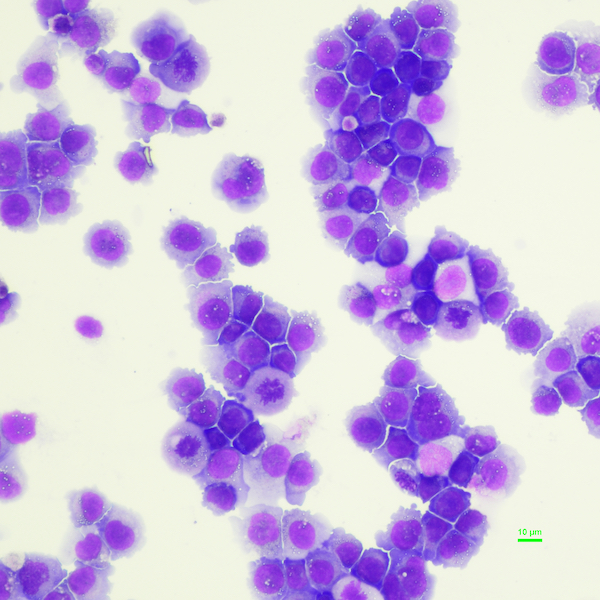
Projects are focused on developing AML models from human blood stem cells and induced pluripotent stem cells. These complementary approaches will yield renewable sources of ‘leukaemia’ cells for high-throughput studies, enabling the identification of new therapies for children with AML.
Generation of childhood AML models using cord blood stem cells

Generation of iPSCs from relapse refractory childhood AML samples

Immunopeptidomics analysis of childhood AML cells

Dr Carmichael has significantly advanced the development of innovative adult leukaemia models and the understanding of molecular alterations driving inherited and acquired forms of myeloid and erythroid leukaemia. She is now turning that knowledge to childhood AML. View all publications
Related childhood cancers: Acute myeloid leukaemia (AML)
Technologies: iPSC, CRISPR and drug screening, Immunopeptidomics, leukaemia modelling, gene editing, stem cell isolation and culture, proteomics and genomics.