Mistaken identity: new mechanism behind stomach cancer identified
By Hudson Institute communications
Improved treatments for a range of cancers could be possible following a discovery that stomach cancer is driven by a different process than previously believed.
Hudson Institute of Medical Research scientists hope their discovery will result in more targeted treatment for numerous cancers, including stomach, colon, pancreas, lung, liver, head and neck.
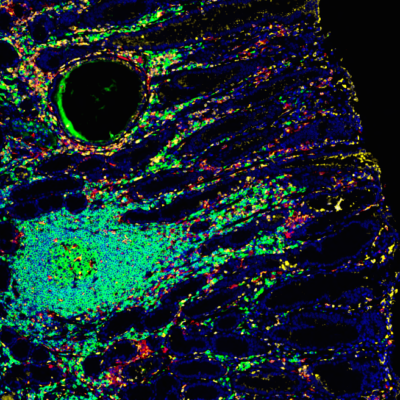
The processes investigated relate to how modifications to protein molecules in our bodies can potentially trigger stomach and other cancers.
They involve a protein generated from the STAT3 gene, which provides instructions for activating a wide range of additional genes that are part of essential chemical signalling pathways within cells, and two amino acids—tyrosine and serine.
Switching cancer on

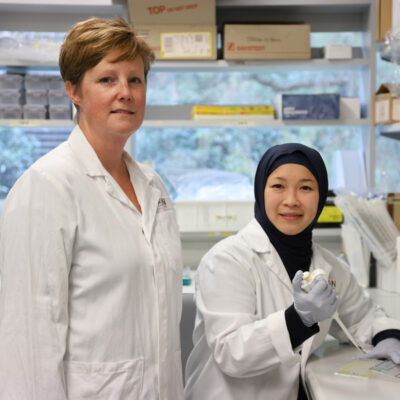
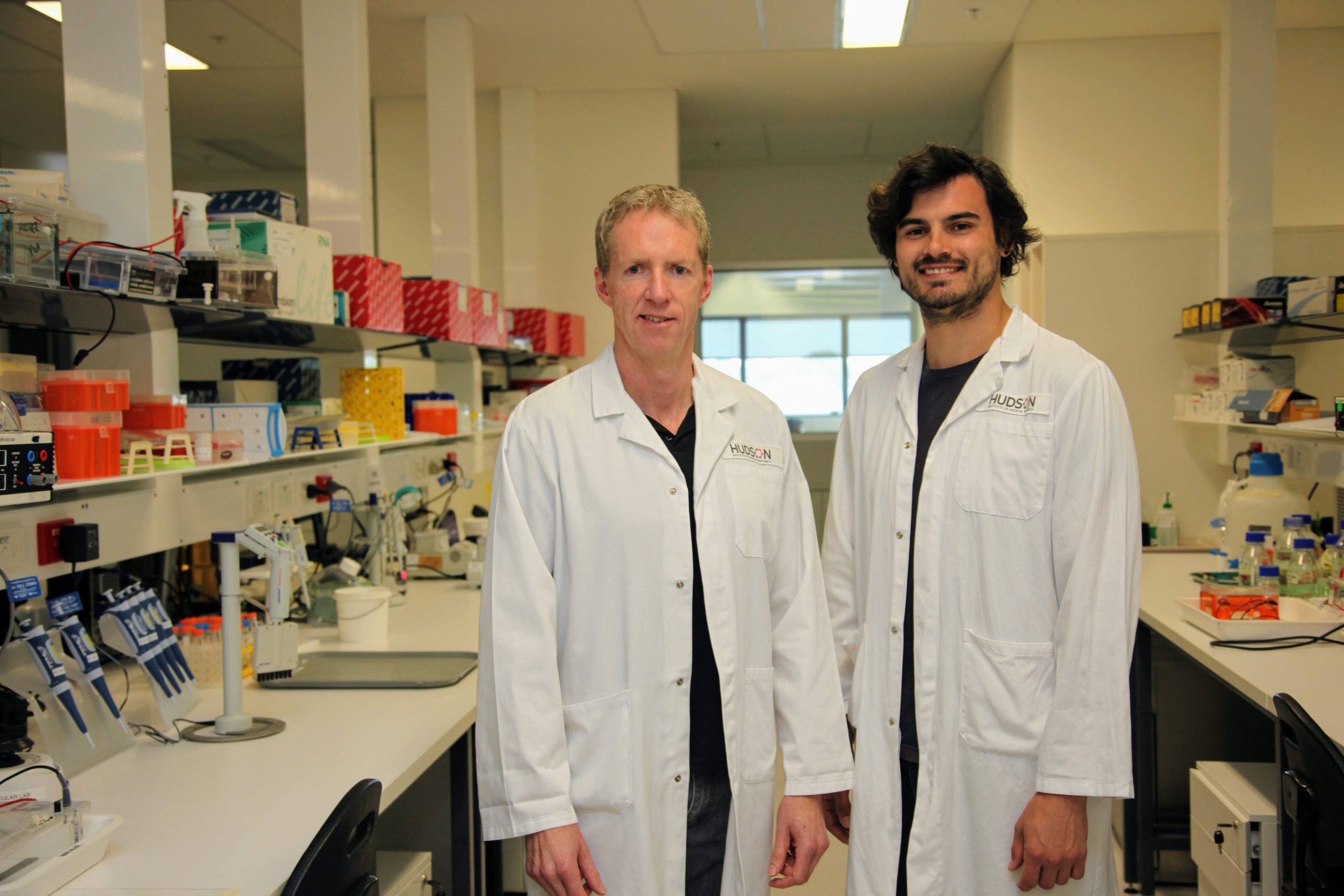
Published in Cancer Research, the Hudson Institute study by PhD student Jesse Balic and Research Group Head of the Cancer and Immune Signalling Laboratory (Hudson Institute), Professor Brendan Jenkins, found for the first time that a form of STAT3 protein modified by a process called serine phosphorylation controlled the production of many other genes that promote stomach cancer.
Up until this study, it had been believed that tyrosine phosphorylation of STAT3 protein, which involves a different amino acid, was the main driver.
Phosphorylation of STAT3 increases its activation, and in turn the expression of many genes that are involved in cancer processes such as cell proliferation.
The research provides new insights into how STAT3 drives stomach cancer and potentially others as STAT3 is linked to at least 50 per cent of cancers.
Blocking cancer-causing agents
Professor Brendan Jenkins, the senior author, says the results could lead to new ways of blocking some cancer-causing pathways.
“Our study shows that efforts to block the actions of STAT3 in cancer should not be against the tyrosine phosphorylated form of STAT3, but rather its serine phosphorylated form,” he says.
“This has the potential to greatly influence the design of future drugs.”

Stomach cancer is the world’s fourth most common. Professor Jenkins says the latest findings could transfer to other cancers in which over-active STAT3 has been implicated, including colon, pancreatic, lung, liver, head and neck.
“STAT3 is in fact thought to be over-active in at least 50 per cent of all human cancers,” he says. “Current strategies to block the actions of STAT3 have been largely ineffective.
“Our study provides opportunities for new strategies to pharmacologically target STAT3 in stomach cancer, and other STAT3-driven cancers such as colorectal and pancreatic, which thus far has been problematic.”
Professor Jenkins says tyrosine phosphorylation does play a role under normal conditions and during disease, but his research found it was not the main driver of cancer.
“Tyrosine phosphorylation still plays an important role to allow STAT3 entry into the nucleus of cells, but serine phosphorylation is essential for the ability of STAT3 to drive the expression of (i.e. turn on) genes once bound to them,” he explains.
Next steps
Professor Jenkins says more research is now needed to design drugs that specifically block serine phosphorylation rather than tyrosine phosphorylation.
He says researchers are already working to develop STAT3 inhibitors for use with chemotherapy to better optimise cancer treatment.
“There are several STAT3 inhibitors currently being used in early phase I or II clinical trials against various cancer types, but the results of such trials haven’t been released yet as they are ongoing,” he says.
If these are successful, such inhibitors could then be tailored to a patient after screening genes for STAT3 activity.
“Standard of care chemotherapy will still be used, but targeting STAT3 with drugs can be used as adjuvant (pharmacological or immunological agent that modifies the effect of other agents) in the context of precision medicine,” Professor Jenkins says.
“It has potential to prolong lives beyond that currently with standard of care chemotherapy.”
Other recent projects involving Professor Jenkins have identified a family of genes that could more accurately detect early stage stomach cancer, investigated diagnosing lung cancer and emphysema earlier and discovered how to inhibit a lung cancer-causing gene.
What are serine phosphorylation and tyrosine phosphorylation?
- Serine and tyrosine are different amino acids in a protein, and phosphorylation is a modification to these amino acids by the addition of a phosphate group, leading to increased activity of that protein.
- Tyrosine phosphorylation of STAT3 was believed to be the main driver of stomach cancer because it is elevated in someone who has cancer and facilitates processes that bind STAT3 molecules together and onto genes which in turn ‘switches on’ cancer cell growth.
- The new study found that serine phosphorylation, which is slightly different, was the main driver of this process.
This research was supported by | National Health and Medical Research Council (NHMRC)
Journal | Cancer Research
Title | Serine-Phosphorylated STAT3 Promotes Tumorigenesis via Modulation of RNA Polymerase Transcriptional Activity
View publication | https://doi.org/10.1158/0008-5472.CAN-19-0974
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”