Breakthrough in diagnosing disorders of sex development
By Rob Clancy, staff writer. Reviewed by Professor Vincent Harley

Disorders/differences of sex development (DSD) are difficult to diagnose because of the multiple phenotypes and genes involved, but a new technique developed at Hudson Institute of Medical Research is set to change all that.
Key points
- New Diagnostic Model: Researchers have developed a technique to reprogram skin cells into testicular cells (Sertoli cells), simplifying the diagnosis of disorders of sex development (DSD) by allowing detailed study and testing without the need for gonadal tissue samples.
- Genetic Insights: This research has identified important genetic targets to advance the understanding of how genetic mutations contribute to DSDs, paving the way for more accurate diagnoses and potential treatments.
Understanding DSD
About one in 5000 babies is born with DSD or intersex, where their genetic, hormonal or physical sex characteristics (genitals, gonads and chromosome patterns) are not typically male or female.
Until now diagnosing the cause of many DSDs has been hampered because the events that determine sex development occur at around week nine of gestation and only in a small number of cells of the gonads of the developing fetus.
But Professor Vincent Harley and his team have developed a model to study this through reprogramming skin cells into testicular cells (Sertoli cells) to understand the changed cell and genetic processes that lead to the Intersex condition in that patient.
“We study the genes involved in formation of the testis in the embryo, but our understanding of this process is limited by the obvious problems in obtaining human samples. So we developed a way of transforming skin cells into the key cells of the testis, the Sertoli cells, which we can then grow and analyse,” he said.
Simpler sex development disorder diagnosis critical
Their research, published in the journal Biology of Sex Differences, shows how this technique can address the lack of availability of gonadal tissue from patients at specific developmental stages by allowing diagnostics tests to be carried out on reprogrammed skin cells.
Prof Harley explains: “Sertoli cells are relevant because they act like an organising centre of embryonic gonadal development and many DSDs arise when these developmental processes go awry.”
“Accurate diagnosis is critical to inform the occurrence of life-threatening crises (e.g. congenital adrenal hyperplasia), the response to hormone replacement therapy, eventual gender identity, cancer risk and counselling for future fertility.”
“Patients suffer a long diagnostic odyssey, with many never receiving a definitive diagnosis,” Prof Harley said. “Our new model will help Identify new causes and mechanisms of DSD in children.”
Finding the genes contributing to sex development disorders
A different but related research paper in Frontiers in Cell and Developmental Biology showed a new target for mutations in and around the SOX9 gene which is likely to contribute to DSDs.
The authors, led by Prof Harley, identified Trpc3, which is a SOX-9 target, and is up-regulated by SOX9. They found that inhibition of Trpc3 expression by Pyr-3 impaired germ and endothelial cell development, suggesting that ‘TRPC3 may mediate SOX9 function during Sertoli, germ and endothelial cell development.
Identifying specific molecular changes
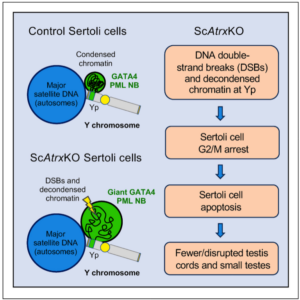
Another significant piece of research from Hudson Institute will lead to greater understanding of the mechanisms by which a particular gene on the Y chromosome, called ATR-X, can lead to genital and testicular abnormalities.
The work, published in iScience, saw the team establish a mouse model with deleted ATR-X gene that recapitulates these defects (G2/M arrest and apoptosis, ie: cell death).
Using this model, they were able to identify the specific molecular changes that result in impaired testis formation and spermatogenesis.
These studies advance our understanding of basic biological mechanisms, and the perturbations that lead to sex development disorders including intersex conditions.
Journal | Biology of Sex Differences
Title | Reprograming skin fibroblasts into Sertoli cells: a patient-specific tool to understand effects of genetic variants on gonadal development
View publication | https://link.springer.com/content/pdf/10.1186/s13293-024-00599-y.pdf
Journal | Frontiers in Cell and Developmental Biology
Title | A role for TRPC3 in mammalian testis development
View publication | https://pubmed.ncbi.nlm.nih.gov/38425503/
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”