Childhood cancer detectives embrace open-source AI solution
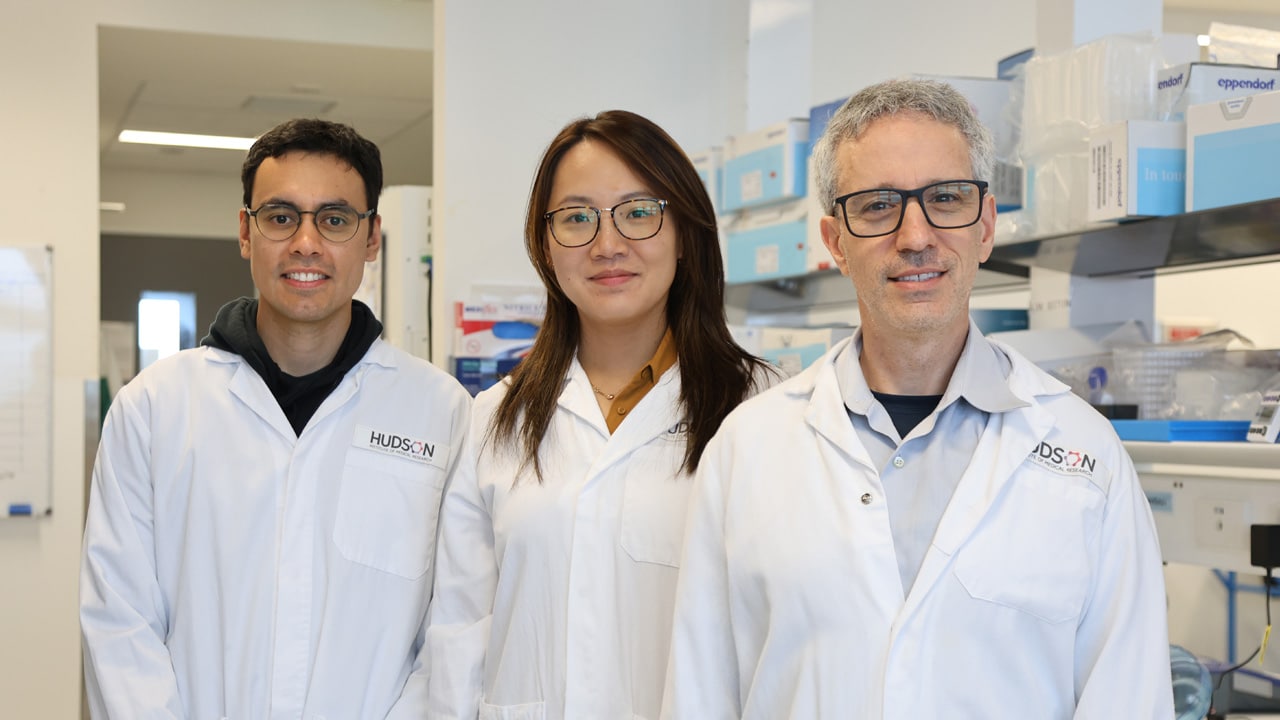
By Rob Clancy, staff writer. Reviewed by Professor Ron Firestein
The old saying goes that a problem shared is a problem halved. In the world of cancer research, there are few problems bigger than paediatric solid and central nervous system (CNS) tumours. These tumours are the number-one cause of childhood cancer-related deaths.
Childhood cancer facts
- 1 in 5 children will not survive
- Most survivors suffer long-term disability from the treatments
- Number one cause of death for Australian children
- 12 cancer drugs approved for children in the last 40 years, compared to 500 approved for adults
Limited drug development for childhood cancers
Exacerbating this problem, the pharmaceutical industry puts little emphasis on developing new drug treatments for kids’ cancers, due to their relatively small numbers compared to adult varieties.
As a comparison, the US Food and Drug Administration (FDA) approved more than 500 adult cancer drugs in the last four decades, but only 12 for childhood cancers, and none for brain or CNS cancers in kids.
“Paediatric cancers are unique from adult cancers, so we don’t necessarily expect the same drug that works in adult cancers to work in children,” said Dr Paul Daniel.
A global solution for children with cancer
Hudson Institute cancer specialists, co leaders in the establishment of the Victorian Paediatric Cancer Consortium (VPCC) Precision Medicine Program, realised that the more this problem is shared, the greater the chances of success.
Faced with such a monumental challenge, Hudson Institute’s Centre for Cancer Research, headed by Professor Ron Firestein, decided to share the burden, bringing highly competitive institutions together in pursuit of a common goal: to accelerate the search for new treatments and cures.
Creating the Childhood Cancer Model Atlas (CCMA)
Together, they created the Childhood Cancer Model Atlas (CCMA), a highly sophisticated paediatric cancer hub offering an open-source bank of childhood cancer tumour tissue samples complemented by advanced artificial intelligence (AI) data-mining tools.
With the world’s largest collection of high-risk paediatric cancer cell lines consolidated in one location, hospitals worldwide now collaborate by sharing tumour tissue samples with Hudson Institute researchers. These researchers utilise the samples for comprehensive testing against a wide array of cancer drugs.
Milestone in paediatric cancer research
That means researchers working anywhere in the world on childhood cancers can have their potential treatments tested then analysed using the latest AI techniques, with the results available for every paediatric oncologist and childhood cancer researcher worldwide.
The story of the CCMA featured in the esteemed journal, Cancer Cell, marking a milestone in paediatric cancer research and embedding Hudson Institute as a global leader in the field.
The role of bioinformatics in cancer research
This work goes way beyond the testing of tissue samples. Dr Claire Sun is a bioinformatician, whose job involves compiling, collating and condensing huge amounts of data, as the team performs hundreds of tests on each tumour type.
“Having models [samples] of various childhood cancers is the only way that we can study the disease and understand how it develops, what makes it grow and ultimately what treatments can be used to fight it off and hopefully cure it,” Dr Sun said.
Insights from global experts on paediatric cancer
“Drs Sun, Daniel and Prof Firestein have addressed the urgent need to develop a childhood cancer cell line resource to identify the vulnerabilities of specific cancers towards improving targeted therapies for paediatric solid and central nervous system tumours. Their work also provides important insights into new targets of clinical relevance for paediatric-focused cancer drug development.”
Professor David Eisenstat, Head of the Children’s Cancer Centre at Melbourne’s Royal Children’s Hospital and Group Leader, Neuro-Oncology, Murdoch Children’s Research Institute.
“Understanding the vulnerabilities of paediatric tumours is essential to help identify new therapeutic approaches. This work is a ‘tour de force’ that includes the largest collection of brain tumour models, generating a resource that will be invaluable to researchers across the world.”
Dr Mimi Bandopadhayay, Assistant Professor of Paediatrics, Harvard Medical School
The potential of combination therapies in clinical trials
Traditional clinical trials often focus on single-agent treatments, but the team recognises the transformative potential of combining multiple drugs concurrently, so their next steps involve leveraging the power of combination therapies for improved paediatric cancer outcomes.
This approach, illustrated through collaboration with the ongoing international phase II clinical trial, CONNECT2109, presents an opportunity for rapid translation of research discoveries to improve outcomes for children with cancer.
“We’re like detectives, creating models that copy how tumours act, looking at all the tiny details and figuring out what could work best. The CCMA is like a treasure trove for researchers and clinicians all over the world, helping us work together to find better ways to help these brave kids,” said Prof Firestein.
The CCMA is the outcome of seven years of support and more than $7 million in funding from the Children’s Cancer Foundation. The CCMA also benefited from the support of the Australian Government’s Medical Research Future Fund and the Robert Connor Dawes Foundation.
Childhood brain cancer: building hope
Virginia’s story
Pippa Rea was just nine years old when she was diagnosed with a diffuse intrinsic pontine glioma (DIPG), a cancerous tumour in the brainstem.
Surgery was too dangerous, so she underwent simultaneous chemotherapy and radiotherapy, which suppressed the tumour for 14 months until it grew again.
The tumour eventually took Pippa’s life 21 months after diagnosis.
Her mother, Virginia, donated the tumour post-mortem for tissue samples, which provided DNA, RNA and a live cell line.
“We never thought of the tumour as part of Pippa and, naturally, wanted it removed. Understanding that the cell line has now become a spider’s web connecting research labs around the world gives us a sense of closure with the tumour and provides us with a positive impact. We will always be advocates for the importance of post-mortem donation but hope that one day we won’t have to be,” said Virginia Rea, mother of Pippa Rea.
Monique’s story
Luca Boggia went from being an active three-year-old to needing extensive brain surgery in a matter of weeks, due to what turned out to be an extremely rare cancerous tumour.
Eleven rounds of chemotherapy and 33 consecutive days of radiotherapy later, he was on his way back to health.
Luca has just had his ninth birthday and his mother Monique Boggia says he’s thriving.
She’s thankful for the opportunity to donate her son’s tumour tissue and hopeful that the next family who finds itself in the same position has an easier time of it.
“I’d hope that through the work of the surgeons and researchers, the next family gets a clearer picture of the available treatments and what can be done,” said Monique, mother of Luca Boggia.
Read more stories like this in the
2023 Annual Report
Collaborators | Nearly 50 collaborations with cancer research institutes, universities and academic medical centres around the globe, including Monash University; QIMR Berghofer Medical Research Institute; Sydney Children's Hospital UNSW; University of Newcastle; Bambino Gesù Children's Hospital (Italy); Children’s Brain Tumour Network (USA); Duke-NUS Medical School (Singapore); Hopp Children’s Cancer Centre (Germany); Johns Hopkins University (USA); KK Women's and Children's Hospital (Singapore); McGill University (Canada); Stanford University (USA); The Children's Hospital of Philadelphia (USA); The Hospital for Sick Children (Canada); The Institute of Cancer Research (UK); University of California San Francisco (USA), University of Lübeck (Germany)
This research was supported by | ALCCRF; Children’s Cancer Foundation; MRFF; MyRoom; NHMRC; Robert Connor Dawes Foundation; VCA
Journal | Cancer Cell
Title | Generation and multi-dimensional profiling of a childhood cancer cell line atlas defines new therapeutic opportunities
View publication | https://www.cell.com/cancer-cell/fulltext/S1535-6108(23)00080-6
In this article
- Childhood cancer facts
- Limited drug development for childhood cancers
- A global solution for children with cancer
- Creating the Childhood Cancer Model Atlas (CCMA)
- Milestone in paediatric cancer research
- The role of bioinformatics in cancer research
- Insights from global experts on paediatric cancer
- The potential of combination therapies in clinical trials
- Childhood brain cancer: building hope
- Virginia’s story
- Monique’s story
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”








