Local discovery + global collaboration = STI breakthrough
By Rob Clancy, staff writer. Reviewed by Professor Paul Hertzog
A discovery at Hudson Institute more than 20 years ago is still sparking new medical insights, with researchers at a major US University using it to uncover vital facts about sexually transmitted disease (STI).
A team at UMass Chan Medical School used an Australian-developed mouse model to test their theory that Interferon Epsilon (IFNε) plays a crucial role in the presence of gonorrhoea – opening the door to potential treatments and more.
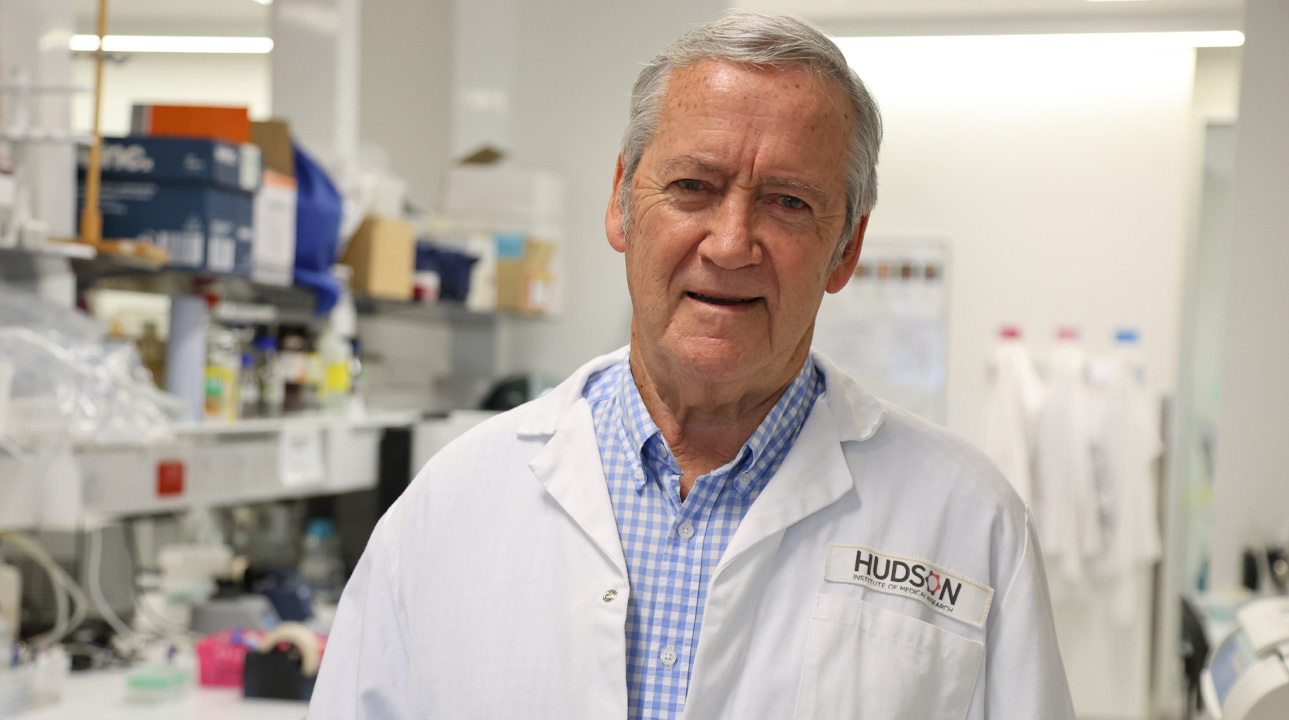
Professor Paul Hertzog discovered IFNε in 2004, and since 2013, when he first identified its function, he and his team at Hudson Institute of Medical Research have shown that it acts as a natural booster of immunity to infections, with potential uses in treating a range of conditions including ovarian cancer and endometriosis.
He explains that it also subject to hormone regulation: “ IFNε is stimulated by estrogen and inhibited by progesterone, but we also showed that it has a protective effect in models of progesterone-dependent STI infections (HSV, Zika, Chlamydia).”
This led to an interesting discussion with Professor Douglas T. Golenbock, MD, the Neil and Margery Blacklow Chair in Infectious Diseases and Immunology at UMass Chan Medical School: “His model of gonorrhoea infection was estrogen-dependent and we wondered if the opposite would happen – IFNε would enhance gonorrhoea infection – and it did.” Prof Hertzog said.
His collaboration with this research extended to providing his own reagents – knockout mice that cannot make IFNε, the recombinant IFNε his team made here in Melbourne and antibodies to detect it and neutralise it.
Results confirmed their theories
“Instead of protecting against infection, in this instance IFNε facilitates infection with Nyceria gonorrhoeae,” Prof Hertzog said. “In the battle between hosts and pathogens, this is a new way for pathogens to subvert the host defence. “
“This pathogen uses an IFNε -dependent metabolic pathway to avoid other anti-bacterial systems.”
This opens the way for the development of gonorrhoea treatments that target the IFNε -dependent metabolic pathway to avoid other anti-bacterial systems.
But Prof Hertzog believes these findings offer wider benefits: “This study represents the discovery of IFNε ‘s involvement in this metabolic pathway which might have implications for its role in cancer and mucosal physiology in general.”
It’s a 21-year-old discovery that keeps on giving.
About gonorrhoea
History
- Ancient origins: Gonorrhoea has been documented since ancient times, with references in Greek and Roman texts; the name comes from Greek gonos (seed) and rhoia (flow), mistakenly thought to be semen discharge.
- Identified pathogen: In 1879, German physician Albert Neisser discovered the bacterium Neisseria gonorrhoeae, confirming it as the cause of the disease.
Causes
- Bacterial infection: Gonorrhoea is caused by the bacterium Neisseria gonorrhoeae, which infects mucous membranes of the reproductive tract, rectum, throat, and eyes.
- Transmission: It spreads through unprotected vaginal, anal, or oral sex with an infected person, and can also be passed from mother to baby during childbirth.
Effects
- Symptoms: Common symptoms include painful urination, genital discharge, and pelvic pain; however, many cases—especially in women—can be asymptomatic.
- Complications: If untreated, it can lead to serious health issues like pelvic inflammatory disease (PID), infertility, and increased risk of HIV transmission.
Treatments
- Antibiotics: Gonorrhoea is typically treated with antibiotics, though resistance to common drugs (like penicillin and ciprofloxacin) has made treatment more challenging.
- Dual therapy: Current guidelines often recommend dual antibiotic therapy (e.g., ceftriaxone and azithromycin) to combat resistant strains and ensure effectiveness.
About UMass Chan Medical School
UMass Chan Medical School, one of five campuses of the University of Massachusetts system, comprises the T.H. Chan School of Medicine, the Morningside Graduate School of Biomedical Sciences, the Tan Chingfen Graduate School of Nursing, ForHealth Consulting at UMass Chan Medical School, MassBiologics, and a thriving Nobel-Prize-winning biomedical research enterprise. UMass Chan is advancing together to improve the health and wellness of our diverse communities throughout Massachusetts and across the world by leading and innovating in education, research, health care delivery and public service. It is ranked among the best medical schools in the nation for primary care education and biomedical research by U.S. News & World Report. Learn more at www.umassmed.edu.
Collaborators | UMass Chan Medical School, Evelyn A. Kurt-Jones, Sunita Gulati, Michael King, Rosane B. de Oliveira, Peter A. Rice, Bo Zheng, Jutamas Shaughnessy, Jennifer L. Edwards, Sanjay Ram, Douglas T. Golenbock
Journal | Cell Host & Microbe
Title | Interferon-epsilon, an estrogen-induced type I interferon, is uniquely exploited by Neisseria gonorrhoeae via effects on sialic acid metabolism
View publication | https://www.sciencedirect.com/science/article/pii/S1931312825001982?via%3Dihub
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”