Next-generation degradable 3D meshes to repair POP
By Rob Clancy, staff writer. Reviewed by Dr Kallyanashis Paul

A debilitating condition affecting one in four women is desperately crying out for a solution, and the next generation of treatments to repair the damage of pelvic organ prolapse (POP) has just come a big step closer.
POP develops when tissues, pelvic floor muscles and ligaments that support the pelvic organs (bladder, uterus and bowel) are damaged, usually in childbirth. This injury causes the organs to shift, or ‘drop’, into the vagina or even outside of the body, often with debilitating results.
It has been described as a hidden pandemic affecting 25 per cent of all women and 50 per cent of post-menopausal women.
Chronic POP requires surgical reconstructions but there are few safe options to repair the damage.
The surgical use of synthetic, non-degradable meshes has been banned since they were found to be responsible for serious and life changing damage in a significant number of patients, so Hudson Institute researchers have spent recent years developing a safer alternative, that works with a woman’s body, not against it.
Breakthrough in repair options
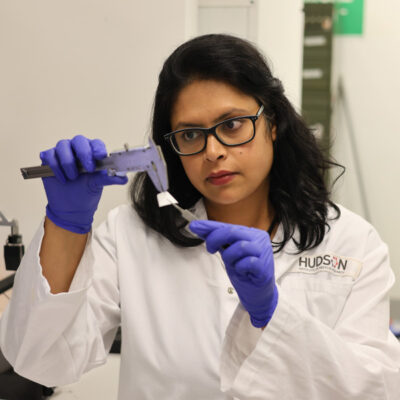
The latest study by Hudson Institute researchers, Dr Kallyanashis Paul and Group Head, Associate Professor Shayanti Mukherjee, fabricated degradable meshes to regenerate vaginal tissue using a polymer material approved by the US Food and Drug Administration (FDA) to create tissue engineering therapies for treating POP.
This world-first study developed alternative degradable melt electrowrite (MEW) vaginal implants for transvaginal pelvic floor reconstruction, presenting a ground-breaking research angle for treating POP via advanced 3D printing methods.
Dr Paul’s specialist knowledge of 3D printing technology was key to the success of the project, which has just been published in the Advanced Science journal.

Next generation repair solutions
“This study identified the simple geometrical attributes, namely, angle and porosity, to regenerate damaged tissue following childbirth injuries,” Dr Paul said. “Using layer-by-layer addition 3D printing technology, nine architecturally different meshes were fabricated to optimise the architecture that will allow the mesh’s degradation while boosting tissue integration.”
“One of the major issues caused by previous meshes was chronic foreign body response (FBR), which degenerates the vaginal tissue from re-growth. We have used preclinical models to test the various design factors required to make a mesh that the body will accept, not reject.”
This study points the way for creating the next-generation of alternative meshes.
Boosting native tissue repair
A/Prof Mukherjee said: “This study provides hope by developing customisable meshes that can boost native tissue repair, so the body will eventually reabsorb the mesh, leaving healthy new tissue and reversing the damage that POP can cause.”
Veteran stem cell biologist Professor Jerome Werkmeister is equally enthusiastic.
“We already know that our eMSC therapy (treatment with Mesenchymal stem cell (MSC)-derived extracellular vesicles) can modulate the immune response to mesh implantation,” Prof Wermeister said.
“This research has found that the mesh geometry itself is also critical and can be designed and fabricated to promote tissue integration by orchestrating a favourable immune response. We believe this will enhance our endeavours towards clinical translation and hopefully commercialisation.”
What is POP?
POP is a condition, often caused by injuries during childbirth, in which muscles and tissues that support pelvic organs become weakened, leading to one or more of these organs dropping from their original position into the vagina.
POP is essentially a hernia through which organs protrude because supporting tissue is weak. This can lead to debilitating symptoms, including poor bladder or bowel control and pain during sex.
The condition can be exacerbated by age, ethnicity, multiple births, obesity and family genetics. One in five women require surgery – and often multiple surgeries.
Transvaginal meshes were banned in Australia in 2017, mainly due to the excessive stiffness resulting in penetration through the vagina into other organs, and undesirable foreign body response to synthetic non-degradable meshes which led to serious complications in some women.
There is an urgent need for safe, effective POP treatments.
This research was supported by | 1. International Postgraduate Research Training and Monash Graduate Scholarships (K.P.) 2. Hudson Institute of Medical Research; Science and Industry Endowment Fund (Grant no. PF16–122 CG, JW, AR for SM) 3. CSIRO Clayton Australia 4. National Health and Medical Research Council (NHMRC) of Australia (Grant IDs 1184841 (SM, JW), 1173882 (CG), 1159677 (CG, SM, JW); 5. Johnson and Johnson WiSTEM2D scholar’s program (SM); 6. Medical Research Future Fund (MRFF) (CIA KP); 7. Rebecca L Cooper Foundation and the Victorian Government's Operational Infrastructure Support Program (SM).
Journal | Advanced Science
Title | 3D Printed Mesh Geometry Modulates Immune Response and Interface Biology in Mouse and Sheep Model: Implications for Pelvic Floor Surgery
View publication | https://doi.org/10.1002/advs.202405004
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”