Research transforming pelvic organ prolapse treatment
By Rob Clancy, staff writer. Reviewed by Associate Professor Shayanti Mukherjee
It’s the most common medical condition you’ve never spoken about.
A condition affecting 40 per cent of all women, to varying degrees.
A condition that costs the Australian healthcare system $200 million each year.
A condition that can leave sufferers with drastically reduced quality of life – unable to run, play with or even lift their kids – and STILL it is rarely, if ever, discussed in public forums.
Pelvic Organ Prolapse (POP) is as old as motherhood itself and is crying out for contemporary solutions.
Courage and advocacy: Sally Maconochie’s journey
It takes courage to speak about your experiences with POP and a special kind of courage to put your face and your name to this very personal condition.
Sally Maconochie has that kind of courage and more – and, ironically, she has the silence of previous generations to thank.
Three years after giving birth, this once fit and active woman found herself recovering from vaginal repair surgery that had an 80 per cent chance of failure, when her mother told her that she had a prolapse and so did her grandmother.
No-one in her family had ever mentioned prolapse and, despite all her research on how best to prepare for childbirth, she had never encountered any information about the risk of POP, let alone how to avoid it.
“POP impacts an enormous number of women around the world,” Sally said. “The critical thing is that nobody talks about it. I want to see real solutions before, during and after childbirth. That’s why I am talking about it to anybody who will listen!”
Following her surgery Sally reached a low point, realising she would never be as physically able as she was before childbirth – that she might never be able to dance, run or walk with her little boy.
“I was so angry that nobody had told me all the ways I could have helped to prevent prolapse and birth injury – I was facing a life of immobility that could have been prevented.”
Out of her anger and desperation Sally chose to do something positive – she is now Hudson Institute’s first POP Advocate.
“I want to spread the word about prevention and I’m working to raise funds for research, in the hope that one day no other women will find themselves in this position.”
World-leading POP science
POP facts
- 1 in 4 women globally in their 40s live with POP
- 1 in 2 women over 50 years of age live with POP
- $200 million annual cost to the Australian healthcare system
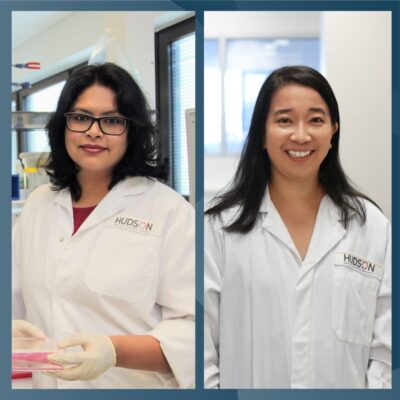
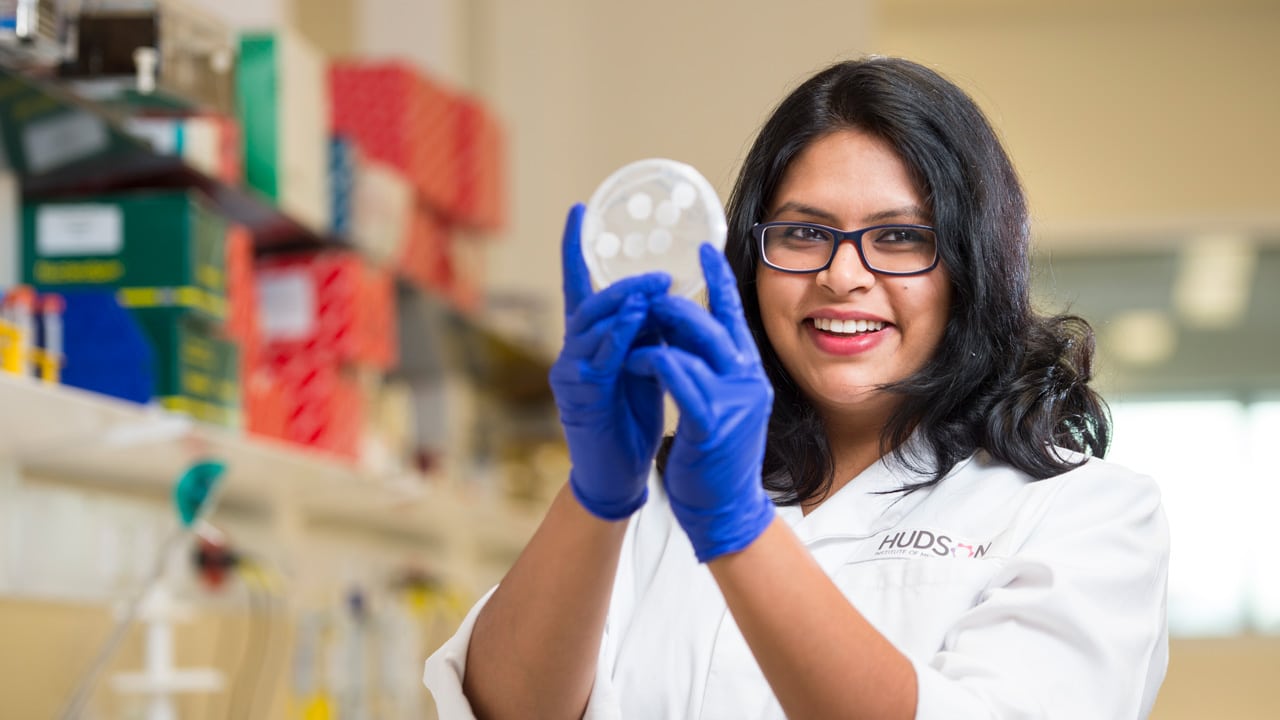
Dr Shayanti Mukherjee, Head of Hudson Institute’s Translational Tissue Engineering lab, specialises in innovative cell-based therapies for pelvic floor disorders and birth trauma injuries.
“There is no adequate treatment for POP and no treatment that can prevent its onset following a vaginal birth injury,” said Dr Mukherjee. “So, women suffer in silence for years to decades, with new solutions desperately needed to improve their quality of life.” Dr Mukherjee brings a unique 21st century skillset and a fierce determination to this challenge, with a PhD in nanostructured biomaterials and a commitment to advancing women’s health utilising biomedical engineering.
“A defining moment in my career was learning that my materials engineering and nanotechnology background could change the lives of women,” she said. Her research merges multiple disciplines to understand how chronic pelvic floor disorders manifest after childbirth injury and she applies her knowledge to develop novel cell-based tissue-engineered therapies for pelvic reconstruction to
advance maternal urogynaecological health.
“My vision is to break this impasse for women by introducing new paradigms in pelvic reconstruction that will reduce suffering due to birth injury,” said Dr Mukherjee.
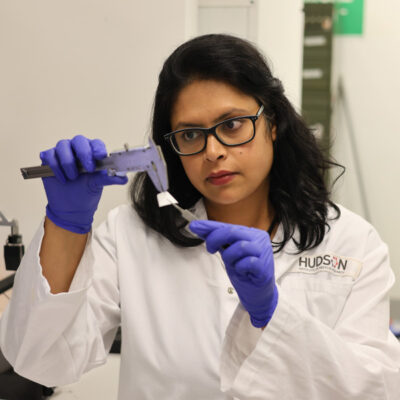
Revolutionary treatment approaches: 3D-printed degradable mesh
Dr Mukherjee’s research uses a woman’s own stem cells to create a 3D-printed degradable mesh, promising to avoid the complications that have plagued previous synthetic non-degradable meshes.
The aim is a simple one – a one-step safe and effective surgical treatment for POP, providing hope for millions of women worldwide.
“By integrating cutting-edge techniques like electrospinning and 3D printing of materials and cells, I aim to revolutionise maternal urogynaecological health, offering transformative solutions and improving the wellbeing of women affected by this prevalent issue.”
“This research has the potential to revolutionise therapies for pelvic floor regeneration and enable personalised medicine for women,” she said.
Prevention and cure: a holistic approach
Dr Mukherjee’s research is as much about prevention as a cure. She is also developing an understanding of how chronic pelvic floor disorders develop after a childbirth injury and improving awareness of birth injuries among obstetricians and midwives.
“We have discovered that early therapy, given soon after childbirth, can heal signs of birth injury and prevent prolapse later in life, giving hope that women will not have to suffer in silence for years,” she said.
A remarkable year
Dr Mukherjee describes her achievements in 2023 as significant – not just scientific milestones but a beacon of hope for herself, her team and all women. Among the highlights were the granting of nearly $4 million in research funding for her POP research, including a Victorian Medical Research Acceleration Fund Grant, an NHMRC Ideas Grant and a Rebecca L Cooper Foundation Fellowship. Dr Mukherjee also gained valuable industry experience with pharmaceutical and biotechnology company, Moderna, during a six-month full-time fellowship with the company.
“Without this funding, we could not take this research further. Taking it further means bringing these new techniques from the lab, through pre-clinical trials and eventually into the clinic, potentially benefitting millions of women,” she said.
A future of hope and health for women
“By advancing innovative cell-based therapies, we are on the brink of transforming the landscape of maternal urogynaecological health, promising a brighter and healthier future for women across the globe,” said Dr Mukherjee.
“It represents a leap towards a future where groundbreaking research transforms healthcare, ensuring better lives and equitable wellbeing for our community.”
Keep up-to-date with critical pelvic organ prolapse research: sign up for the POP newsletter
Read more stories like this in the
2023 Annual Report
Collaborators | Australian National Fabrication Facility; Monash Health; Monash University
This research was supported by | MTPConnect; NHMRC; Rebecca L Cooper Foundation; VMRAF
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”