Harnessing a natural killer to fight lung cancer
By Rob Clancy, staff writer. Reviewed by Associate Professor Daniel Gough
Making tumours visible to the body’s own natural killer cells could be the key to fighting the deadliest form of lung cancer.
Lung cancer is the leading cause of cancer related deaths world-wide and small cell lung cancer makes up 15 per cent of all new diagnoses. Due its resistance to current treatments and ability to metastasise (spread), only 5 per cent of patients survive.
For over 40 years small cell lung cancer patients were treated with the same ineffective drugs. New treatments that harness the patient’s immune system to fight their lung cancer have changed the playing field, but so-called “cold tumours” such as small cell lung cancer find ways of becoming invisible to the immune system, limiting the utility of these treatments.
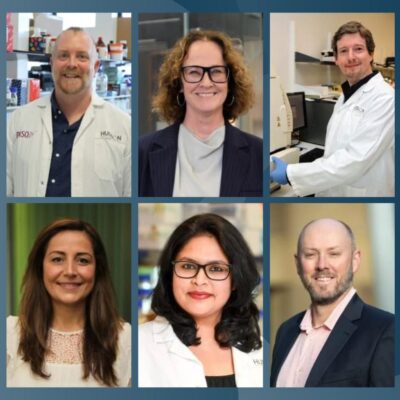
Associate Professor Dan Gough and his team at Hudson Institute of Medical Research are studying how to make these cold tumours visible to the immune system and prevent them spreading to other parts of the body.
He says identifying patients who will respond and enhancing the response in patients who don’t respond to these treatments is the current holy grail.
Harnessing the immune system to help it fight lung cancer
Their research, published in Nature Immunology, highlights the critical role that the innate immune system plays in making tumours visible to the host.
“The innate immune system is often associated with the body’s response to infection. We show that it is also critical for the body to be able to “see” a tumour as it develops. Without this immune visibility tumours rapidly spread.” A/Prof Gough said.
This research, with collaborators from Monash Health, Cancer Care Manitoba and Peninsula Oncology, is the first to link this innate immune regulatory cascade to the metastatic spread of small cell lung cancer.
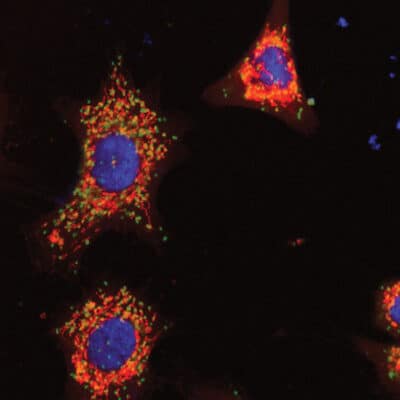
Lead researcher, Dr Aleks Guanizo explained: “We identified a cascade in which the protein STAT3 is essential to maintain the expression of an anti-viral sensing protein called STING. If this cascade is lost then tumours become invisible to the host, allowing for metastasis, which is ultimately lethal.” she said.
Two aspects of this research offer hope for potential new treatments for small cell lung cancer:
- The identification of a specific subset of immune cells called natural killer cells as being essential to survey and limit tumour metastasis.
- We show that the innate sensor pathway that is essential for tumour immunity is not permanently lost and that it can be re-activated by innate immune activating stimuli including the anti-viral molecule interferon.
“This shows the power of a coordinated response engaging both the innate and adaptive immune systems. Importantly, we identify a possible treatment to turn cold tumours hot which will improve patient outcomes,” said A/Prof Gough.
Lung Cancer Facts
- One Australian dies every hour from lung cancer
- Lung cancer is the result of the uncontrolled growth and multiplication of cells in the lung(s) into a tumour.
- Over time, this tumour starts to invade functional parts of the lung, affecting breathing, causing pain and symptoms related to the loss of normal lung function.
- Lung cancer typically doesn’t cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced.
- Smoking is the single biggest risk factor for lung cancer.
- Treatments to fight lung cancer can include surgery, radiotherapy or medicines such as chemotherapy.
Innate immunity explained
The innate immune system is your body’s first line of defence against harmful invaders like bacteria and viruses. It responds quickly and doesn’t need prior exposure to recognize threats.
It incorporates physical barriers, such as skin and mucus, cells like macrophages and neutrophils that “eat” germs, and chemical signals like cytokines that trigger inflammation. It also includes specialised proteins that destroy invaders.
Unlike the adaptive immune system, the innate system is non-specific, meaning it targets a broad range of pathogens without “remembering” them. It acts as a rapid response team, buying time for the adaptive immune system to kick in if needed.
Collaborators | Monash Health, Cancer Care Manitoba, Peninsula Oncology
This research was supported by | Victorian Cancer Agency Mid-Career Fellowship, Cancer Council Victoria, Peninsula Oncology
Journal | Nature Immunology
Title | A Stat3-STING-IFN axis controls the metastatic spread of small cell lung cancer
View publication | https://www.nature.com/articles/s41590-024-02014-5
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”