Natural mesh provides hope for pelvic organ prolapse
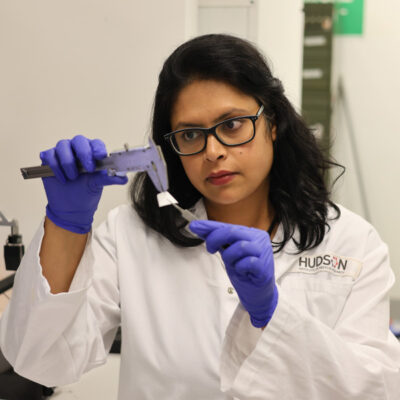
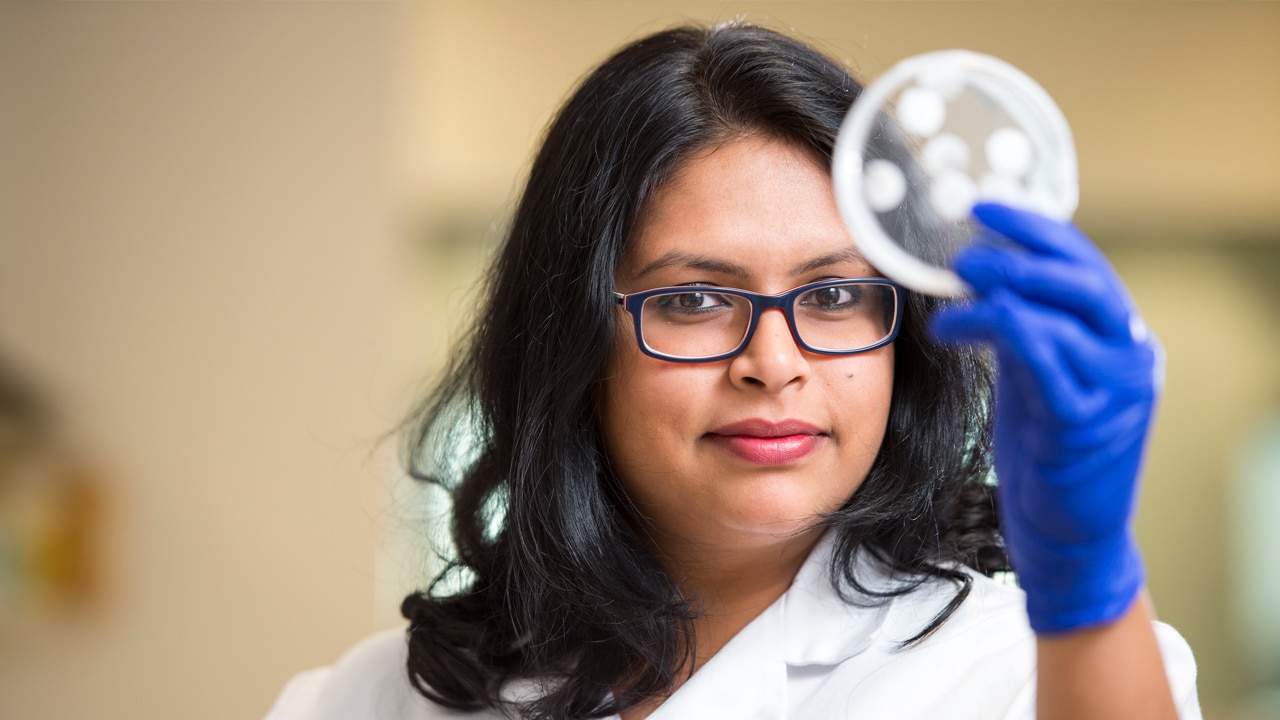
By Hudson Institute communications. Reviewed by Associate Professor Shayanti Mukherjee
A safer and more effective treatment for women with pelvic organ prolapse (POP) may be on the horizon, thanks to a new technique that uses a woman’s own stem cells to boost the effectiveness of a degradable mesh.
What is pelvic organ prolapse?
- POP develops when tissues, pelvic floor muscles and ligaments that support the pelvic organs (bladder, uterus and bowel) are damaged, usually in childbirth. This injury causes the organs to shift, or ‘drop’, into the vagina or event outside of the body. This can lead to debilitating symptoms including poor bladder or bowel control and pain during sex
- POP is a lifelong, potentially debilitating condition. Despite the high prevalence, there is no cure for POP
A study published in Biomacromolecules, led by Dr Shayanti Mukherjee, shows how a degradable mesh, made from a blend of natural and synthetic material and including stem cells from the endometrium, can integrate successfully with the body and enhance the healing process for POP patients.
Essentially, the body treats the mesh as native to the area and not a foreign object. The study shows the body responds positively, enabling the mesh to blend naturally and provide a platform so the stem cells can help to repair the damaged area.
The research shows healing and tissue integration starts as early as one week, with the results more evident around the six-week mark.
Synthetic, non-degradable meshes that have been used to treat POP continue to face severe criticism and litigations. In November 2017, the Therapeutic Goods Administration announced it would remove synthetic vaginal meshes from the register of sale in Australia. Reported complications include chronic pain, infections and the inability to have sex.
“Given that POP affects more than 50 per cent of women aged over 50 years, there is a huge need for a viable treatment. Researchers around the world are looking for better options, degradable meshes being one of them,” Dr Mukherjee said.
“The advantage of this method is that instead of providing a non-degradable mesh to provide the mechanical strength to alleviate POP, we will encourage the body to create its own new proteins to strengthen the vaginal wall.”
Dr Mukherjee said one of the most interesting observations was that the blend of natural and synthetic mesh and presence of stem cells are required for an optimal, long-term response. Therefore, the absence of either element could lead to early degradation of the mesh, resulting in poor healing.
Collaborators | Monash University, Monash Health and CSIRO Clayton
This research was supported by | The CASS Foundation, National Health and Medical Research Council (NHMRC), Rebecca L Cooper Medical Research Foundation, Science and Industry Endowment Fund (SIEF), Youanmi Foundation.
In this article
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”