New male infertility research focuses on sperm formation
By Rob Clancy, staff writer. Reviewed by Professor Kate Loveland
The mysteries of male infertility lie at the heart of many couples’ inability to conceive, however scientists at Hudson Institute of Medical Research have identified a protein which could play a crucial role in the process.
Around one-in-20 couples experiences infertility and in half of those cases, it is due to a problem with the male reproductive system.
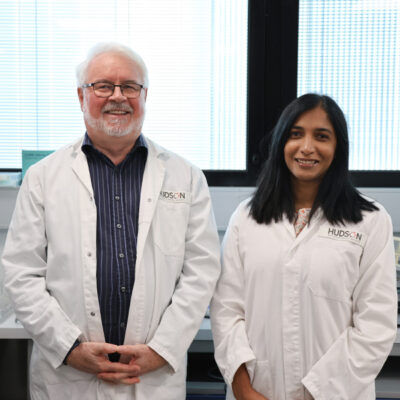
Professor Kate Loveland from Hudson Institute’s Centre for Endocrinology and Reproductive Health, said there is no ‘cure’ for male infertility, but her latest research has pinpointed the essential role that the importin 5 protein (IPO5) plays in sperm formation.
“Although artificial reproductive technologies can be employed to bypass problems preventing normal fertility in some cases, there remains no explanation for between 15 and 30 per cent of cases,” Prof Loveland said.
“Being able to identify possible downstream targets of IPO5 that are required for normal male fertility can help us figure out what the real underlying cause is for many infertile men,” she said.
Mechanisms of testis development and sperm formation
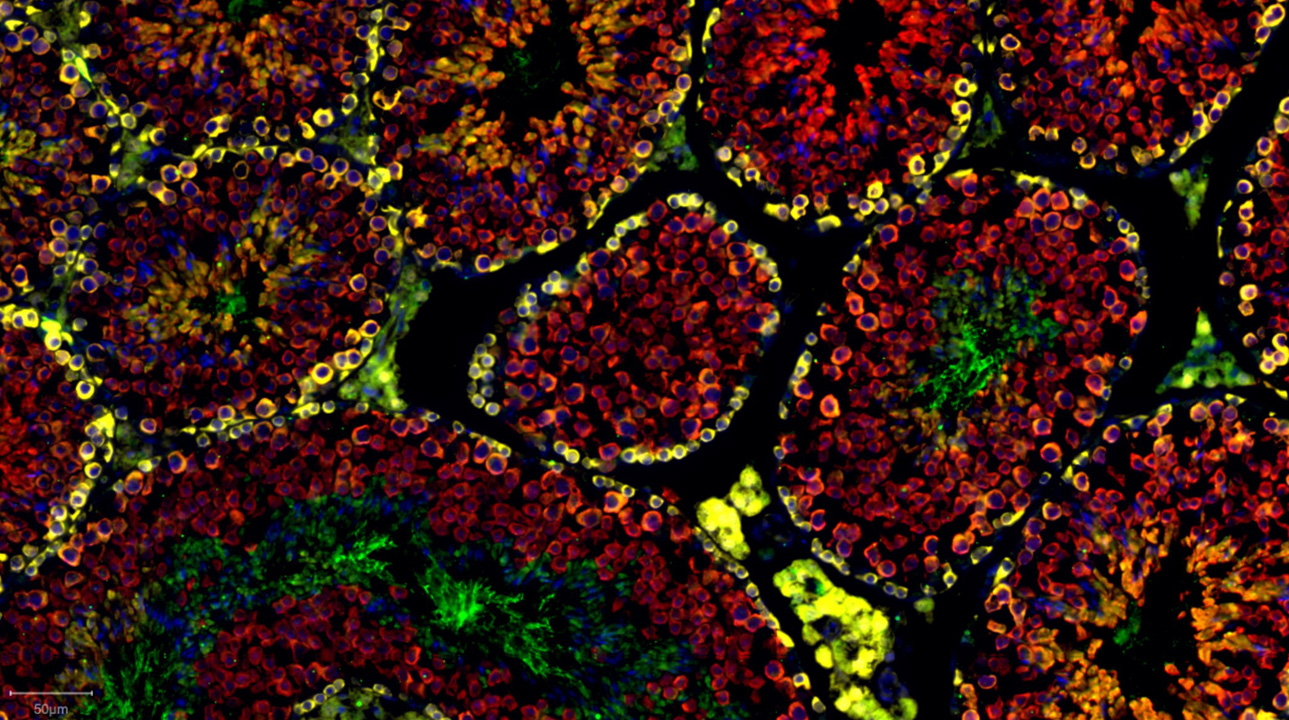
The Testis Development and Male Germ Cell Biology research group, led by Prof Loveland investigates the fundamental mechanisms that underpin testis development, to identify what molecular switches are needed to produce healthy sperm from their precursors, primitive germ cells that first form in the fetus.

That is where IPO5 comes in: this is the first time an importin protein has been implicated as vital for survival of the earliest sperm precursors in mammals, with the identification of its cargo having the potential to explain male infertility.
Its significance is illustrated by the Society for the Study of Reproduction selecting this research paper as its “Editor’s Choice” for the monthly edition of its journal, Biology of Reproduction.
Drs Julia Young and Penny Whiley led the work on this project. A key to this discovery was the use of Hudson Institute’s unique mouse model which was developed through a collaboration spanning three Australian research institutions.
Male infertility facts
Successful male reproduction depends on
- Producing healthy sperm Essential for fertilisation.
- Achieving erection and ejaculating Necessary for delivering sperm to the female reproductive tract.
- Adequate sperm count and motility Crucial for successful fertilisation.
- Normal sperm morphology Impacts the sperm’s ability to fertilise the egg.
Male infertility can result from various factors, including
- Blockages Obstructions in sperm transport pathways.
- Sperm production issues Low sperm count (oligospermia), absence (azoospermia), poor motility, or abnormal morphology.
- Functional problems Erectile dysfunction or ejaculation difficulties.
- Inflammatory conditions STIs or other illnesses affecting reproductive organs.
- Immunological disorders Immune system targeting sperm cells.
- Injuries Trauma to reproductive organs.
- Chronic health conditions Diabetes, obesity or hormonal imbalances.
- Medications Including certain drugs, alcohol and anabolic steroids.
- Environmental factors Exposure to toxins and endocrine-disrupting chemicals.
- Genetic factors Chromosomal abnormalities or inherited disorders.
- Lifestyle factors Stress, poor diet and lack of exercise.
Men should consult a doctor if they
- Have been unable conceive after one year of regular, unprotected intercourse.
- Experience erection, ejaculation problems or other sexual function issues.
- Notice a pain or a lump in the testicle area.
- Have a history of testicular, prostate, or sexual difficulties.
- Are over 35 and have been trying for six months.
- Have a known history of fertility problems.
How can men improve fertility?
Men can enhance fertility by
- Maintaining a healthy weight
- Eating a balanced, nutritious diet
- Reducing stress
- Exercising regularly
- Getting enough sleep
And avoiding
- Smoking
- Excessive alcohol consumption
- Excessive caffeine intake
- Recreational drugs or anabolic steroids
- Untreated STIs
- Heat stress to the testicles (from tight clothing, prolonged sitting or placing laptops on the groin)
- Exposure to pesticides and toxins
- Certain medications (consult a healthcare provider)
- Overtraining or excessive exercise
Collaborators | Mark Baker, Jessie Sutherland and Eileen McLaughlin, University of Newcastle and Hunter Medical Research Institute David Jans, Monash University Cathryn Hogarth, LaTrobe University
This research was supported by | Australian Research Council Centre of Excellence and Discovery Project Grants NHMRC Fellowships
Journal | Biology of Reproduction
Title | The nuclear transport factor IPO5 revealed as a critical mediator of male germline development
View publication | https://doi.org/10.1093/biolre/ioaf134
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”