Collaborative study gives hope to women suffering in silence
By Hudson Institute communications

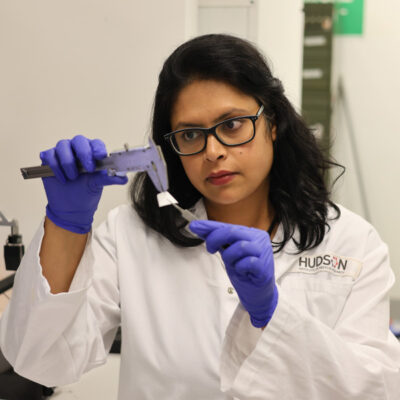
New treatment for millions of women affected by a hidden condition, pelvic organ prolapse (POP), will be the focus of Dr Shayanti Mukherjee’s novel bioengineering project, thanks to a prestigious John Stocker Postdoctoral Fellowship.
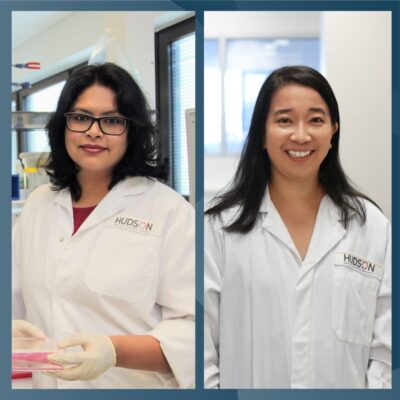
The highly competitive Science and Industry Endowment Fund (SIEF) John Stocker Postdoctoral Fellowship was awarded to Associate Professor Caroline Gargett and Dr Jerome Werkmeister from Hudson Institute of Medical Research and Monash University’s Ritchie Centre; CSIRO Manufacturing, and Dr Anna Rosamilia from Monash Health to train Dr Mukherjee for her project “Bioengineering Novel Nanobiomaterial based Cellular Therapies for the Prevention of Childbirth Induced Pelvic Organ Prolapse”.
A debilitating but hidden condition affecting one in five women, Pelvic Organ Prolapse (POP) commences during pregnancy and childbirth and exacerbates with ageing and obesity.
“At present, millions of women worldwide suffer from POP with very limited treatment options,” said Dr Mukherjee, from Hudson Institute and Monash University’s Ritchie Centre.
“POP is associated with sexual, bladder, and bowel dysfunction, including incontinence that profoundly affect the quality of life and daily functioning of sufferers; in Australia, more than $200 million was spent on urinary incontinence in 2009.”
In the last decade, pelvic support using surgical meshes (primarily synthetic) has been heavily employed with reports of successful outcomes.
However, the US Food and Drug Administration (FDA) issued Public Health Notifications in 2008 and 2011 due to significant and unacceptable mesh-related complications, leading to the withdrawal of several brands of surgical meshes from the market.
Dr Mukherjee said there are currently no clinical trials on cell-based therapies for POP incorporating surgical implants in or outside Australia.
“With the elderly population expected to double by 2030, POP is expected to become more prevalent without any reliable treatment options, representing a significant health and economic challenge for Australia and world-wide,” added Dr Mukherjee.
To address this major health challenge, Dr Mukherjee’s project will develop new biocompatible surgical constructs for the prevention and treatment of POP.
“Dr Mukherjee’s project aims to develop new hydrogels based on self-assembling peptides for delivering mesenchymal stem cells to the vaginal walls or pelvic floor muscles to prevent women developing pelvic organ prolapse,” A/Prof Gargett, head of the Hudson’s Endometrial Stem Cells research group, said.
“Until now, the use of extracellular matrix (ECM) mimicking nanobiomaterials has never been explored for POP,” said Dr Mukherjee.
“My project will also develop new viable secondary prophylaxis for postpartum women to prevent POP and long term surgical treatment options for women with POP.
“Dr Mukherjee will accelerate the clinical translation of these materials and will drive the project through novel study design, experimentation, data analysis, student supervision, new surgical skill development, conference presentation in our new Monash Health Translational Precinct,” said Associate Professor Gargett.
“I will be able to bring together three different fields (stem cell biology, nanotechnology and clinical work in gynaecology) and develop a solution to POP, while receiving mentoring from experts in all three fields and contributing to the research excellence of Hudson Institute and Monash University’s Ritchie Centre,” said Dr Mukherjee.
“POP is a hidden burden—women don’t talk about it, they suffer in silence,” said Dr Mukherjee. “This fellowship signifies support and interest in Australia to improve women’s quality of life.”
The highly competitive SIEF Award provides a 3 year Fellowship for just six postdoctoral fellows each year across Australia covering all scientific disciplines. For 2015 there were 179 applicants.
“The goal of the John Stocker Fellowship is to train highly competitive scientists within three years of postdoctoral experience to become independent researchers at the completion of the Fellowship,” added Associate Professor Gargett, who is also Postgraduate Co-ordinator, Department of Obstetrics and Gynaecology at Monash University.
“Dr Mukherjee’s Fellowship experience in The Ritchie Centre and CSIRO environments will provide her with an excellent foundation on which to launch her future career as a research leader in Australia.”
This important project is a collaborative study involving researchers and clinicians from CSIRO, Hudson Institute and Monash University’s Ritchie Centre and Monash Health.
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”