Pankind backs Hudson Institute immunotherapy research for pancreatic cancer
By Rob Clancy, staff writer. Reviewed by Associate Professor Pouya Faridi
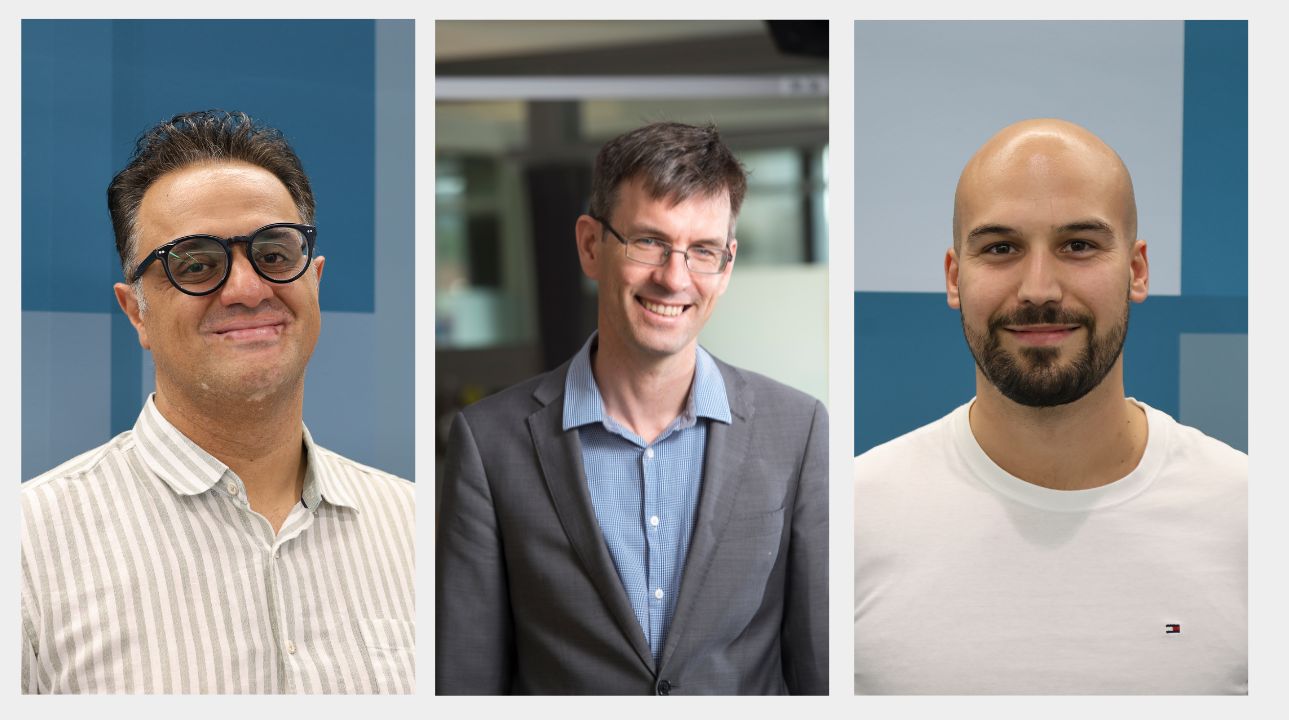
Associate Professor Pouya Faridi has been named among some of Australia’s top cancer researchers to receive funding for his work on immune therapies for pancreatic cancer.
Pankind is the only Australian organisation solely dedicated to improving outcomes for people affected by pancreatic cancer and today it announced $2.5 million in funding for research into the disease, with A/Prof Faridi receiving $100,000 in the New Treatment Innovation category.
His project, titled Exploiting Shared Cancer Antigens for Off-the-Shelf Immunotherapy in Pancreatic Cancer, involves testing a new kind of vaccine that teaches your body’s defence cells—called immune cells—to spot and destroy cancer.
He says current treatments involve tailoring a specific cancer vaccine for each individual patient, but he is taking an alternative approach.
Taking a different path on pancreatic cancer
“Our project takes a different path. Instead of tailoring a shot for every patient’s tumour, we hunt for signs that nearly all pancreatic cancers share,” A/Prof Faridi said.
“If we find one or two shared markers, we can make a single vaccine for lots of people. We’d produce it in big batches, store it on the shelf and ship it when needed—much faster and cheaper than a custom shot.”
A/Prof Faridi and his team, including Dr Dan Croagh from Monash Health and Dr Gabriel Goncalves from Hudson Institute of Medical Research thanked Pankind for providing the desperately needed funding which keeps vital research like this going.
His research focusses on a molecule called HLA-G, which he says is like as a tiny display stand on each cell.
“Healthy adults have almost none of it, but many pancreatic tumours light up with HLA-G, so it’s a clear bullseye for our immune system,” he said.
“Here’s how we do it in the lab: we grow pancreatic cancer cells and collect the tiny protein pieces that HLA-G displays. Those bits—called peptides—act like wanted posters for immune cells. We record which peptides keep popping up on different lab samples.”
Designing pancreatic cancer vaccines
“Next, we test patient tumours to prove that the same peptides appear there. Spotting the same peptides in real tumours shows they’re true cancer markers, not just lab oddities. With that list of shared targets, we design a vaccine that trains immune cells to recognise them.”
He believes a universal, “one-size-fits-many” pancreatic-cancer vaccine could then be administered immediately, avoiding the long wait for a custom version.
“Big clinical trials would be simpler, and far more patients could get help quickly,” he said.
“In the end, this approach could make treatment safer, more powerful and available to many more people—offering hope and saving lives.”
It’s an exciting prospect, made possible by the generous support of Pankind.
Collaborators | Monash Health
This research was supported by | Pankind 2025 Research Grant program $100,000
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”







