Pelvic organ prolapse prevention and cure
By Rob Clancy, staff writer

They say prevention is better than cure, but when it comes to pelvic organ prolapse, the specialists at Hudson Institute of Medical Research are taking them equally seriously.

Pelvic organ prolapse (POP) is a hidden condition affecting up to 50 per cent of women and causing symptoms such as vaginal bulge or a dragging sensation, and bladder, bowel, and sexual dysfunction, as well as severely impaired quality of life.
No reliable POP treatment
There is a currently no reliable treatment for POP, but Hudson Institute’s Translational Tissue Engineering Research group, headed by Dr Shayanti Mukherjee, is working to help those women already experiencing the condition and those whose birth injuries leave them susceptible to it.
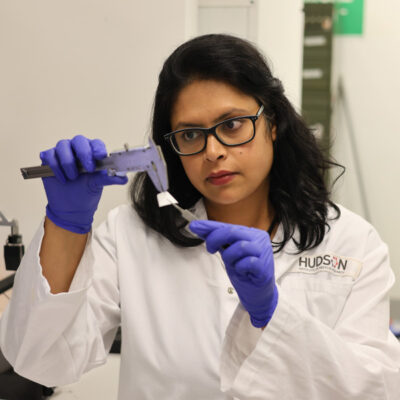
Researcher Dr Kallyanashis Paul is producing excellent results with his project using 3D printing to develop pelvic mesh products from a woman’s own cells.
The use of transvaginal mesh implants has a troubled history, with many patients previously experiencing complications and side effects, but by using a woman’s own cells, Dr Paul hopes to develop mesh which would be better tolerated than existing products.
“I have shown that bioprinted 3D degradable construct is a promising new alternative, which can be significantly improved by bioprinting,” Dr Paul said. “However, this needs a robust “bioink” that can print and retain cells with their therapeutic value intact.”
He was recently shortlisted in the Victorian Premier’s Awards for Health and Medical Research, and is currently studying overseas as part of a veski fellowship, allowing him to undertake international study and advance his 3D printing work in a global setting.
Preventing POP before it develops
At the same time, as well as her own work on new mesh technologies, Research Group Head, Dr Mukherjee, is also using stem cells in a very different way, with the aim of preventing POP before it develops.
POP is frequently the long-term result of injuries sustained by mothers during birth, and Dr Mukherjee’s research involves using stem cells in a gel which can be applied soon after birth to treat these injuries in their earliest stages.
“Although birth trauma injuries occur during childbirth, their impact is often seen much later in life – often after menopause – when women start developing symptoms,” Dr Mukherjee said.
“What is really fascinating about this work is that we can potentially use a woman’s own stem cells from her endometrium, delivered in a natural plant-based gel, to heal her tissue injury,” she said. Through studying the before and after of POP, Hudson Institute is working to prevent this condition ever developing, and to make life easier for the many women in whom it does.
Hudson News Winter 2022
Collaborators | Monash University, Melbourne Centre for Nanofabrication (MCN)
This research was supported by | International Postgraduate Research Training and Monash Graduate Scholarships, The CASS Foundation Medicine/Science Grants, Johnson and Johnson, NHMRC, Victorian Government Operational Infrastructure Support Program, veski Fellowship
About Hudson Institute
Hudson Institute’ s research programs deliver in three areas of medical need – inflammation, cancer, women’s and newborn health. More
Hudson News
Get the inside view on discoveries and patient stories
“Thank you Hudson Institute researchers. Your work brings such hope to all women with ovarian cancer knowing that potentially women in the future won't have to go through what we have!”